Vitamin K2 Puts Calcium in Bones and Removes Calcium From Arteries
Vitamin K2 & Healthy Bones
For decades calcium has been the go-to dietary supplement for improving bone health. However, several studies show that supplementing with calcium exclusively is not enough. The body needs to optimize the use of calcium, making sure it is directed to and utilized by the bones.
Osteoporosis is a disease characterized by loss of bone mineral density. According to the World Health Organization (WHO), osteoporosis currently affects some 200 million people globally. Worldwide, one in three men are expected to suffer from osteoporotic fractures in the future, whereas lifetime risk of fracture for women is nearly one in two. Women are more vulnerable due to two factors:
- Women in general have less bone mass than men
- The annual loss of bone mass in women accelerates after menopause.
Vitamin K2, particularly in the menaquinone-7 (MK-7) form, has been shown to help the body to optimally use calcium by binding it to bones, keeping them dense and strong, and lessening risk of fracture throughout aging.
How is Bone Affected by K2?
Bone is comprised of a hard outer shell and spongy inner tissue matrix, which is a living substance, and the entire skeleton is replaced approximately every 7 years. This process is regulated by osteoblasts (cells that build up the skeleton) and osteoclasts (cells that break down the skeleton). As long as the bone-forming activity (absorption) is greater than the bone-breakdown (resorption), the process of maintaining healthy bones is kept under control.
Osteoblasts produce a vitamin K2-dependent protein called osteocalcin, which helps bind calcium in the bone matrix, leading to increased bone mineral content. Consequently, the skeleton becomes more resistant and less susceptible to fracture. But osteocalcin needs vitamin K2 to function optimally.
In the case of long-term vitamin K2 deficiency, osteoclasts will remove more bone tissue than osteoblasts can build. This will result in a slow and steady loss of bone tissue, eventually leading to porosity, degradation, and weakness of the bones, which could lead to increased risk of fracture.
Studies Show Vitamin K2 Maintains Bone Health
Because natto (the traditional Japanese dish made of fermented soybeans) is the most abundant source of vitamin K2 as menaquinone-7 (MK-7), population-based studies have shown that in those regions in Japan where women consumed the most natto, the women generally have shown low rates of fractures. More observational studies suggest that natto may dramatically reduce risk of developing osteoporosis. Until 2012, there had only been 2, 1-year studies of K2 as MK-7 and bone status in healthy elderly. In these, the MK-7 significantly improved the “switching on” of osteocalcin to get to work (also called OC carboxylation).
Based on these studies, a 3-year study of a vitamin K2 as MK-7 ingredient on 244 women showed for the first time clinically statistically significant protection of the vertebrae and the hip (femoral neck) against osteoporosis. This was achieved with only 180 mcg daily of vitamin K2, which is considered a “nutritional dose,” meaning it is much more easily obtainable through supplementation and the right diet than pharmaceutical doses used in previous studies. The K2 group showed significantly increased circulating active osteocalcin (cOC), a well-established biomarker for bone and vitamin K status. Additionally, the inactive protein, ucOC, in the supplement group decreased with 51% +/- 21 % as compared to the placebo group (+4 % +/- 49%).
After 3 years of supplementation, improvements in both bone mineral content and bone mineral density were statistically significant in the vitamin K2 group. Further, bone strength was statistically improved, demonstrating therapeutic benefits for the K2 group as compared to the placebo group. This study appears in the January 2013 issue of Osteoporosis International, validating the credibility of the research findings.
Vitamin K2 & Children’s Health
Today’s children may be challenged as they grow into adulthood. Diets of convenience (and chemicals) may be severely compromising their bone development and cardiovascular health. Such diets are also devoid of adequate vitamin K2, which clinical trials have shown to protect against bone loss/preserve bone density and strength, and to also protect against dangerous arterial calcification, which can lead to compromised heart health.
Bones are most active growing and developing during childhood. But the habits of childhood carry one into adulthood, and it is possible that cardiovascular arteries could begin to stiffen through calcification as early as childhood. The one common denominator is calcium. Children’s diets are high in calcium as many foods are fortified with this mineral. But calcium that is not properly utilized may stray from binding to bones and instead be deposited into arteries, turning into a rigid, cement-like plaque over time.
The ability to bind calcium to healthy bone matrix maximizes bone mineral density in order to maintain bone mass later in life. The ability to ensure that calcium is inhibited from the arteries promotes enduring heart health.
A Necessary Nutrient
Vitamin K2 is one nutrient children need that provides healthy longevity. The function of vitamin K2 is unique among other vitamins. It activates certain proteins in the body, such as osteocalcin in the bones, Matrix Gla Protein (MGP) in the arteries, and clotting factors in the liver. Osteocalcin is responsible for binding calcium to the bone matrix. Without adequate vitamin K2 intake, a significant portion of osteocalcin will stay inactive and unable to bind calcium. At the same time, MGP helps prevent circulating calcium from adhering to and remaining in arterial walls – provided there is enough vitamin K2 in the body.
Without adequate vitamin K2, specifically as menaquinone-7 (MK-7), calcium cannot be adequately processed in the body to build healthy, strong bones. During childhood and adolescence, bones are highly active and osteocalcin levels are 8 to 10 times higher compared to adult bones – therefore, children require much higher levels of vitamin K2. Unfortunately, many children are vitamin K2 deficient, so supplementing with vitamin K2 should be considered.
Studies Demonstrate Need for Vitamin K2
Population-based studies and clinical trials have clearly linked better K-vitamin status in children to the creation of strong and healthy bones. A 2008 published study showed that improving vitamin-K status in children over a 2-year period resulted in stronger and denser bones. One year later, the same group of researchers demonstrated that in healthy, pre-pubertal children, modest supplementation with vitamin K2 as MK-7 increased osteocalcin carboxylation (activating inert osteocalcin).
In a 2013 published study, researchers tested 896 blood samples collected from 110 healthy volunteers, a group composed of 42 children and 68 adults. The researchers took measurements of biomarkers reflecting the volunteers’ vitamin-K2 status by measuring both circulating inactive MGP and inactive osterocalcin – proteins specific to heart and bone health, respectively. The researchers found that those children and adults with the most pronounced vitamin K2 deficiency showed the highest responses to supplementation with MK-7. Children (and adults above the age of 40 years) showed the largest vitamin K2 deficiency, and accordingly may benefit from MK-7 supplementation to improve their vitamin K2 status.
Increasingly, leading medical and nutritional experts strongly recommend that food manufacturers enrich their products with vitamin K2, giving children an alternative to vitamin K2 supplements.
Vitamin K2 Shown to Reduce Cardiovascular Disease Risk
Globally, cardiovascular diseases (CVD) are responsible for nearly 1 in 3 deaths. CVDs typically develop over decades, characterized by arteries that clog and harden from plaque deposits in which calcium is the main mineral component.
The Matrix Gla Protein (MGP) is recognized as the most potent inhibitor of vascular calcification today – studies show that it can inhibit, and even reverse, induced vascular calcification. But MGP is dependent upon vitamin K2 to fulfill its role.
While it was believed that calcification is an unfortunate and inevitable consequence of aging, recent studies demonstrate that arterial calcification is an actively regulated process. Healthy arterial tissues have been shown to contain 100 times more vitamin K2 than calcified arteries – meaning that one can actively protect their cardiovascular system by obtaining adequate vitamin K2.
Vitamin K2 Shown to Reduce CVD Risk
The Rotterdam Study (2004) showed that high dietary intake of vitamin K2 – but not K1 – has a strong protective effect on cardiovascular health. This population-based study, which took place over a 10-year period, included 4,807 men and women 55 years of age or older at the start. Findings from the study indicate that eating foods rich in natural vitamin K2 (at least 32 μg per day) reduces the risk of both arterial calcification and cardiovascular disease by as much as 50% – with no undesirable side effects.
The Rotterdam findings were confirmed in 2008 by another Dutch population-based study investigating the protective effect of vitamin K2. The Prospect study by Gast et al included 16,057 women, and after 8 years of follow-up, vitamin K2 was found to decrease the risk of coronary heart disease (CHD) by 9% for every 10 μg vitamin K2 consumed. The scientists found that the strongest correlation was seen in cases of intake of the higher menaquinones (MK-7, MK-8, and MK-9). Vitamin K1 intake was not significantly related to CHD.
Further, a 2012 double-blind, randomized, clinical trial evaluated the results of a 3-year regular intake of a 180 mcg daily dose of vitamin K2 menaquinone-7 (MK-7) by a group of 244 healthy post-menopausal Dutch women, randomly assigned to receive daily either vitamin K2 or placebo capsules. The trial showed substantial benefits in preventing age-related stiffening of arteries resulting in increase of the PWV (pulse wave velocity) in the placebo group, but not in the vitamin K2 group. Most remarkably, the vitamin K2 group showed it not only prevented stiffening, it also resulted in an unprecedented statistically significant improvement of vascular elasticity both measured with ultrasound techniques and PWV.
Vitamin K2 & Blood Thinners
The mechanism by which blood-thinning medications work inhibits vitamin K. Vitamin K1, due to its ability to support healthy blood clotting, may interact or interfere with anti-coagulants such as warfarin. Researchers concluded in one study that vitamin K2 as MK-7 supplementation at doses as low as 10 μg (lower than usual retail dose of 45 μg) significantly influenced anticoagulation sensitivity in some individuals. Thus, the researchers recommended avoiding use of MK-7 supplements if on vitamin K-antagonist therapy.
However, it has been shown that patients on oral anti-coagulant therapy who take up to 50 mcg of MK-7 per day have more complete activation of osteocalcin without interfering with the effect of the blood thinner. In other words, taking a small amount of MK-7 allows one to avoid the side effects of these medications without interfering with their intended benefits.
On the basis of the latest insights and in order to remain on the safe side, it is recommended that patients on conventional blood thinners consult with their doctor before taking a K2 supplement, since taking more than 50 mcg of K2 might interfere with the prescription.
An interview with Dr. Leon Schurgers
By Richard A. Passwater, Ph.D.
Dr. Stephen Sinatra greatly increased my interest in vitamin K2 during our recent series of interviews. When Dr. Sinatra mentioned in our June 2007 chat that vitamin K2—but not vitamin K1—could reduce harmful calcium deposits from arteries, that was it. I had to learn even more. When I read the research reports of Dr. Leon Schurgers and saw his dramatic illustration of the effect of vitamin K2 on arterial calcification (Figure 1), I knew this was indeed an important breakthrough in treating cardiovascular disease. So, I called upon vitamin K researcher, Dr. Leon Schurgers. Dr. Schurgers was kind enough to share his thoughts on the functions of vitamin K, discuss the significance of new research findings and comment on the potential implications for clinical practice for us. Since February is Heart Month, we will focus largely on the cardiovascular system, but also discuss skeletal health.
We will discuss the “calcium paradox,” by which so many people are having harmful calcium deposits form in their arteries at the same time that calcium content of the bones is decreasing. This calcium paradox is not a result of too little calcium in the diet, but of too little vitamin K2 that largely controls where the calcium goes. The objective is to keep calcium in our bones, not in our arteries. This is the role of vitamin K—putting calcium in its place!
As most of our readers know, but few in the general public know, the amount of calcium that circulates in the blood is rigorously under hormonal regulation. The amount of calcium in the blood is critical to such functions as the heart beat, muscle contraction, vasodilatation and nerve transmission so the level of calcium is under hormonal regulation. If the diet is low in calcium, the parathyroid hormone will increase the blood level of calcium by facilitating calcium removal from the skeletal tissues. Our readers understand that bone is active, dynamic, living tissue, not calcium chalk. On the other had, calcitonin (a hormone produced by the parafollicaular cells [C cells] of the thyroid gland) acts to decrease calcium concentration when levels are high.
Vitamin K functions as a coenzyme during the activation of a number of proteins involved in blood coagulation, bone formation and keeping blood vessels free of calcium. This “activation” is achieved by vitamin K assisting the production of a “carboxylated” form of these proteins.
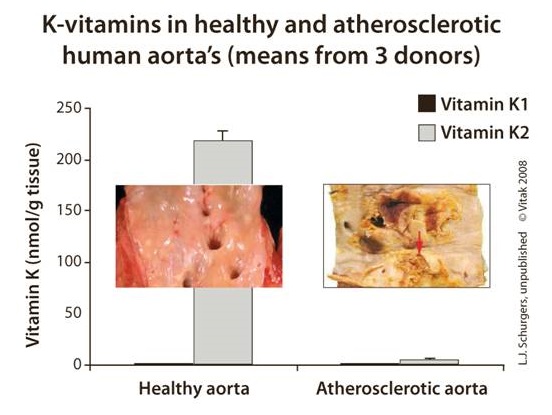
Figure 1: Photo of vitamin K2-deficient and vitamin K2-nourished aortas. Note that the aorta on the left has adequate levels of vitamin K2 and is free of calcium deposits, whereas the vitamin K2 deficient aorta on the right is highly calcified. Photo courtesy of Dr. Leon Schurgers.
Vitamin K has been known as the “coagulation vitamin” since its discovery, which is usually credited to the Danish scientist, Dr. Henrik Dam in 1929. The letter “K” used to designate the vitamin is from the German word Koagulationsvitamin. Through the years, it has been found that vitamin K is not a single compound, but a family of compounds having similar chemical structural features. There are two main sub-families within the vitamin K family.
Within the past three decades, the essential role of K vitamins in maintaining bone and cardiovascular health have become known as a significant amount of research has published. Not only do the K vitamins play an important role in forming blood clotting proteins in the liver, the K vitamins are required for the proper functioning of the proteins such as the three bone-mineralizing proteins (especially the Gla-protein osteocalcin) and the widely distributed calcification-inhibiting matrix Gla protein (MGP) that keeps calcium out of arteries.
It is especially important to note that Western populations are vitamin K-deficient for optimal bone and heart health. Even if peopleconsume sufficient vitamin K to ensure proper blood clotting, larger amounts are necessary to sustain bone and blood vessel health, particularly in aging adults. It is also interesting to note that much of the vitamin K research is done by groups in the Netherlands, where the population consumes a diet considerably higher in vitamin K than the U.S. population.

About Dr. Leaon Schurgers:
Dr. Leon Schurgers is a senior scientist in biochemistry at the Maastricht University in The Netherlands. He is vice president for VitaK Research at the Maastricht University, the world’s largest research institute dedicated to vitamin K. Furthermore, as a senior scientist for the Division on Vitamin K Research, Dr. Schurgers is part of the Cardiovascular Research Institute, the largest research institute of the University of Maastricht. Dr. Schurgers’s major occupation is leading the scientific part on vitamin K research and supervising technical engineers, post-docs and Ph.D. students. Dr. Schurgers is a member of the American Society of Bone and Mineral Research, the International Society on Thrombosis and Haemostasis as well as the American Heart Association. He has published over 50 research papers in the international scientific press.
Passwater: What led you to become a biochemist?
Schurgers: As a child I had many questions, always related to “how” and “why.” I guess my scientific instinct was already present at a young age. Also, during my education, the human body and how life develops, works and sometimes fails always fascinated me. I find it continuously fascinating and very satisfying intellectually. Biochemistry is the “Chemistry of Life,” where we are able to take advantage of recent progress in knowledge and to translate them into health benefits and solutions. Being central to all sciences, biochemistry gives us the opportunity to utilize this knowledge for the benefit of all.
Passwater: Why did you research vitamin K? After all, until now, it hasn’t been a sexy vitamin to study.
Schurgers: When I started my career at the Maastricht University, our group was part of the Cardiovascular Research Institute Maastricht (CARIM). Thus, we all worked on vascular disease. My interest was focused on MGP, a vitamin K-dependent inhibitor of arterial calcification. It intrigued me that this inhibitor could be modulated: its activity depends upon vitamin K! At first sight, nobody was interested in calcification, as it was regarded as a passive process, always present in diseased arteries. It was not thought to be of clinical importance then. Now, calcification is regarded as one of the most predictive values of vascular disease, and vitamin K plays a major role.
Passwater: We’ll get back to the role of MGP later. How did vitamin K2 get into your research picture?
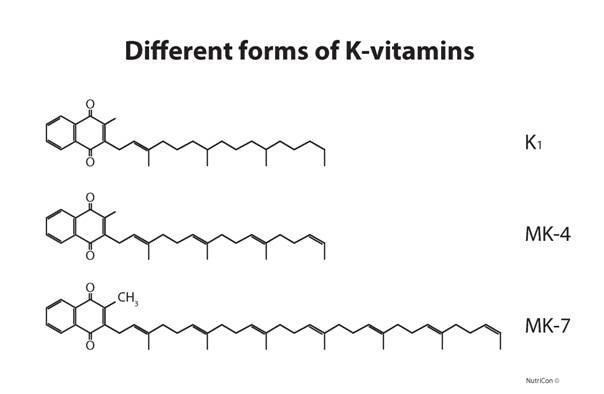
Schurgers: As two natural sub-families of vitamin K are known, designated as K1 (phylloquinone) and K2 (menaquinone), they needed further evaluation. Because of their dissimilarity in chemical structure, these two sub-families of vitamin K have different bioactivities, efficacies and bioavailabilities, which impact the way they function within the body. Figure 2 shows the chemical structures of the two vitamin K sub-families.


Figure 2: The two primary sub-families of naturally occurring vitamin K: vitamin K1 (phylloquinone) and vitamin K2 (menaquinone). The vitamin K family members are 3-substituted 2-methyl-1,4 naphthoquinones. Phylloquinone (top structure), a form originating in plants contains a phytyl group; “long-chain” menaquinones (bottom structure) (MK-n), originating primarily by bacteria in the lower bowel, contain a polyisoprenyl side-chain with 6 -13 isoprenyl units in the 3-position. A specific menaquinone, MK-4, is not a major bacterial product, but can be formed from menaquinone and phylloquinone. Of course, animal products can contain both forms. Additionally, there are important members of each sub-family as shown in Figure 4 (in part 2 of this article).
During my Ph.D. process I studied the bioavailability and bioactivity of each form. We found that vitamin K1 goes primarily to the liver, and only a small amount is released for the periphery, whereas vitamin K2 is equally distributed over our body, via the redistribution in the liver in VLDL and LDL particles via the blood. Therefore, vitamin K2 can be of great importance for peripheral tissues such as the arterial vessel wall.
Passwater: Very interesting. Please elaborate more on why our readers should care about vitamin K2.
Schurgers: While K1 is poorly absorbed and has little influence on cardiovascular health, K2 has a beneficial effect on both bones and vasculature. In the nutritional (physiological) dosage range, natural vitamin K2 provides the source of vitamin K preferred by extrahepatic tissues, including bone, cartilage and soft tissues. Vitamin K2 prevents arterial calcium accumulation, which is associated with the development of cardiovascular disorders. I believe our research is having a very good impact on vitamin K usage in general, which is particularly important when vast the vitamin K deficiency in the Western population is taken under consideration.
Passwater: Keeping calcium out of our arteries and in our bones certainly is a great take-home message. The need for K2 in keeping calcium in bones seems straightforward, but how did you elucidate the fact that vitamin K2 can remove calcium from arteries?
Schurgers: We have shown that cardiovascular disease and osteoporosis have some common pathways and elements. Studies carried out during the last decades showed that calcium can be definitively linked to the two diseases. In laymen’s terms, this is put forward as the “Calcium Paradox” (see Figure 3): while lack of mineral in the bones makes them weak, excessive amounts of calcium in blood vessels makes them more rigid, leading to hypertension and subsequently cardiovascular disease

The first clues that vitamin K2 is important for cardiovascular health came from the so-called “Rotterdam Study.” In this prospective study, healthy elderly people consuming the highest intake of dietary vitamin K2 had some 50% less vascular calcification and cardiovascular death. Thus, the link between vitamin K2 consumption and vascular disease was established. This work has now been confirmed by a second, independent study showing the same trend.
Passwater: Does this apply to reversing calcium accumulation in the arteries as well as halting further accumulation of calcium in arteries over time?
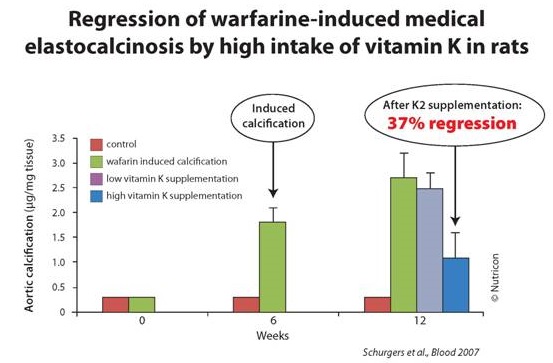
Schurgers: Yes indeed! At least that’s the hypothesis we put forward. The Rotterdam Study gave us the clue for in which direction to look. We found out that MGP acts as a strong inhibitor of vascular calcification. MGP was shown to be the strongest inhibitor of arterial calcification, which fully depends for its functionality on vitamin K. We have tested this in experimental animals and it was shown that vitamin K2 could fully protect against warfarin-induced arterial calcification and even could reduce existing vascular calcification by 37%.
These latest findings on the importance of vitamin K2 intake may mean a major advance for the treatment of cardiovascular diseases, as our experiments gave evidence that vitamin K2 supplementation is capable of not only stopping, but also reversing the effects of arterial calcification. Before any conclusions can be drawn for humans, we need to study this effect in human clinical trials. However, the results thus far look very promising.
Passwater: We’ll discuss the importance of the warfarin-vitamin K antagonism shortly, but I want to clear up one thing. Are these all animal studies or is there human clinical evidence as well?
Schurgers: The benefits of vitamin K2 on blocking and regressing calcification are indeed animal studies. However, a benefit of vitamin K2 for prevention of cardiovascular disease was shown in the Rotterdam Study. The Rotterdam Study, involving approximately 4,800 people over a 10-year period, revealed that increased dietary intake of specifically vitamin K2 significantly reduced the risk of CHD mortality by 50% as compared to low dietary vitamin K2 intake.
What is more, outcomes of some new studies revealed that patients on hemodialysis (kidney disease) are typified by low protection against arterial calcification due to poor vitamin K status. Also, patients suffering from cardiovascular disease such as aortic stenosis and heart failure showed a poor vitamin K status. In the first pilot results, supplementing dialysis patients with vitamin K2, clearly show a significant benefit of vitamin K2 as menaquinone-7 (Mk-7). If this will lead to less calcification and eventually less death, it needs to be investigated.
I emphasize that the calcification of the arteries seen in chronic kidney disease is the same type of calcification that is found in aging population. The accumulation of calcium in the arteries results in stiffening and increased fragility. This might be considered a silent killer, as hardening of the arteries develops without any symptoms over time. The process of calcification is an actively regulated process and that adequate vitamin K2 intake can prevent this process and potentially reduce this risk factor.
Passwater: Let’s give our readers a break here and come back next month in Part 2 with a discussion of the research showing that nutritional levels of vitamin K2 can reverse calcium deposits in arteries, the effect of vitamin K2 on bone health. How vitamin K works in the body, what are adequate and optimal levels of vitamin K intake and interaction of vitamin K with anti-coagulation medication.
In figure 1, which clearly demonstrates that vitamin K2-deficient aortas calcify whereas adequately vitamin K2-nourished aortas are calcification free. Let’s translate the photograph into numbers. Figure 4 is a graph showing the correlation of vitamin K2 level with decreased calcification of the aorta.
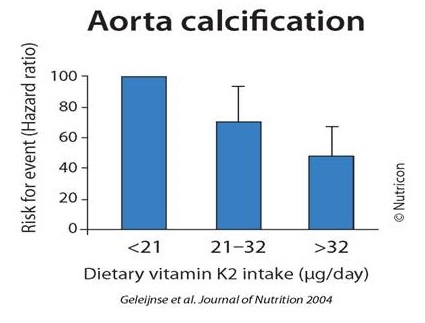
Figure 4: Aorta calcification decreases with vitamin K2 nourishment. Courtesy of Dr. Schurgers.
More importantly, the risk of dying from cardiovascular disease decreases with increasing vitamin K2 levels. Figure 5 clearly shows this relationship.
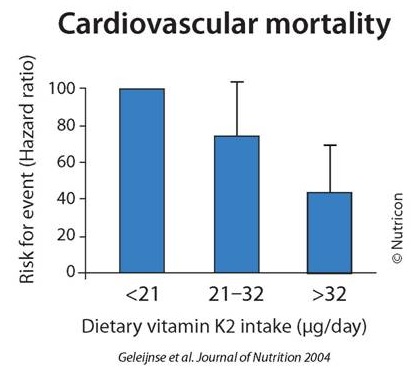
Figure 5: Death due to cardiovascular disease declines markedly with increasing vitamin K2 nourishment. Figure courtesy of Dr. Schurgers.
Passwater: In Part 1, you discussed your research showing that vitamin K2 prevented the calcification of arteries that occurs when warfarin is taken. We’ll discuss the warfarin–vitamin K interaction shortly, but in essence, warfarin induces calcification in arteries as warfarin blocks vitamin K’s ability to activate MGP. Would you elaborate on this study for us?
Schurgers: We use warfarin to experimentally induce arterial calcification. In this study, we gave warfarin to control animals together with vitamin K1 to prevent bleeding. After stopping the warfarin plus vitamin K1 regimen, we continued with high vitamin K2 supplementation. Figure 6 shows the results graphically. Vitamin K2 reduces the arterial calcification caused by the warfarin. This is a good model to demonstrate how vitamin K2 reduces arterial calcification due to a vitamin K2 shortage.
Passwater: Can calcium accumulation reversal be achieved with nutritional levels of vitamin K2? Currently, there is no RDA for vitamin K as the Food and Nutrition Board of the Institute of Medicine is of the opinion (as of 2001) that there is only sufficient scientific evidence to establish an “Adequate Intake” (AI) of 120 mcg for men and 90 mcg for women. This should be adequate for the activation of the blood-coagulation factors, but I feel that more is needed for optimal bone and artery health. As a note to our readers, the Food and Nutrition Board is a scientific body and is not to be confused with the U.S. Food and Drug Administration’s “US RDA” established in 1973 as a reference for use in nutritional labeling and other regulations involving nutrition components. The US RDAs are set based on the Food & Nutrition Board’s recommendations, but in the case of vitamin K, the FDA appears woefully out of date.
Schurgers: For the general healthy population, natural vitamin K2 will be effective in nutritional (physiological) dosages, which fits in the current official recommendations. As Figure 4 shows, the data from the Rotterdam Study nicely show that the regular consumption of 45 mcg vitamin K2 per day reduced the incidence of calcification by 50%.
Passwater: Do these nutritional levels present a problem to people on anticoagulation medication? Oral 4-hydroxycoumarin derivatives such as warfarin are widely prescribed anticoagulants for the treatment of thrombotic disorders. Warfarin is also commonly used as a rodent poison as large quantities can cause them to bleed to death. These drugs inhibit the body’s cycling of vitamin K to the active form that assists in the gamma-carboxylation of specific proteins such as procoagulants, osteocalcin and GMP. Earlier, you mentioned inducing arterial calcification by using warfarin.
Schurgers: Today, we find daily intakes of 45 mcg vitamin K2 do not interfere with anticoagulation medication. It is known that the high intake of vitamin K (either K1 or K2) overcomes the anticoagulant effect of coumarins. As long as coumarins such as warfarin are around, interference with vitamin K (whatever form) will be an issue. I am very confident that most people will switch in the near future from coumarin to specific oral anticoagulants such as dabigatran, which may not be available in the United States yet. Dabigatran has been marketed as Pradaxa since April 2008 in European countries and as Pradax in Canada. For now, we advise people on oral anti-coagulant medication to consult their medical doctors.
Passwater: Interesting! Around Thanksgiving time, a message went out to hospitals to make them in compliance with a national Joint Commission requirement regarding vitamin K-controlled diets for warfarin patients. Most patients on warfarin are warned not to consume “cranberry juice and dark greens such as spinach, broccoli and collard greens.” This advice will have detrimental effects on bones, arteries and heart valves. It is better to consume a constant intake of vitamin K and balance the ratio of warfarin –to–vitamin K with the International Normalized Ratio.
For normal healthy persons, there are no known adverse effects due to doage as vitamin K has no activity other than gamma-carboxylation of certain proteins, and once they are 100% carboxylated, no other action occurs.
Schurgers: The U.S. Food and Nutrition Board of the Institute of Medicine has not set an Tolerable Upper Intake Level as no adverse effect has been reported for healthy individuals consuming vitamin K.
Passwater: What is the difference between vitamin K1 and vitamin K2?
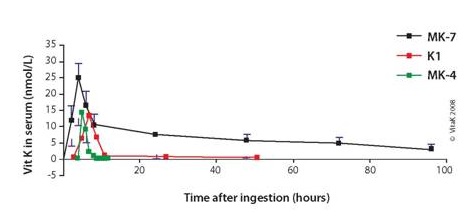
Schurgers: As Figure 2 in Part 1 shows, vitamins K1 and K2 are structurally related compounds exhibiting the same function: activation of vitamin K-dependent proteins. They differ, however, in the side chain and thus in lipophylicity. Because of this difference, vitamins K1 and K2 have different bioactivities, efficacies and bioavailabilities. Our research has shown that due to this difference, vitamin K1 is poorly absorbed (only some 15%) because of its tight binding to the chloroplast membrane. Moreover, vitamin K1 is not redistributed by the liver, and thus its main effect is the activation of vitamin K-dependent clotting factors in the liver. On the other hand, vitamin K2—due to its lipophylic character—is not only used by the liver but also redistributed via blood in VLDL and LDL. Therefore, vitamin K2 is very accessible for extra-hepatic tissues such as bone and vessel wall.
Passwater: What are good natural food sources of vitamin K2?
Schurgers: Vitamin K1 is found in green leafy vegetables, where it is tightly bound to the chloroplast membrane. Vitamin K2 is of bacterial origin. Therefore, we find it in fermented food products, where the bacteria are used as starters fermentation culture. Typical fermented foods are cheese, curd cheese and sauerkraut. The best source of vitamin K2 is the traditional Japanese dish natto. Natto is a fermented soy bean that is very popular in Japan, but not appreciated outside Japan. Now, this special vitamin K2 is available as supplement without any smell and taste. Small amounts of both K1 and K2 can be found in various animal products as animals consume plant-form vitamin K1 and absorb vitamin K2 from their intestinal tracts.
Passwater: Do we need to consume both K1 and K2 or would K2 be able to satisfy all of vitamin K needs?
Schurgers: That is a good question! Since vitamin K2 is taken up by the liver and redistributed in the circulation via LDL, all tissues bearing a LDL receptor can make use of this vitamin. This includes bone, vasculature and liver. Moreover, due to its very long half-life in the circulation (> 3 days), it is available for all tissues 24 hours a day. So, if we take natural vitamin K2, no extra supplemental K1 is needed.
Passwater: You have mentioned matrix Gla protein (MGP) twice. MGP is a protein that carries calcium similar to a chelate that holds calcium “in its claws,” but it doesn’t do this unless the MGP is “activated” by vitamin K. This is a critical finding. What is this all about?
Schurgers: Vitamin K achieves a process on the proteins called “carboxylation.” Carboxylation gives the proteins claws so they can hold onto calcium. Once the protein grabs onto calcium, it can be moved. Gamma-carboxylation is catalyzed by the vitamin K-dependent gamma-carboxylase. If there is not enough vitamin K2 in the blood, then some of the MGP will remain inactive and not able to do its job of putting calcium where it belongs. Figure 7 shows this relationship.
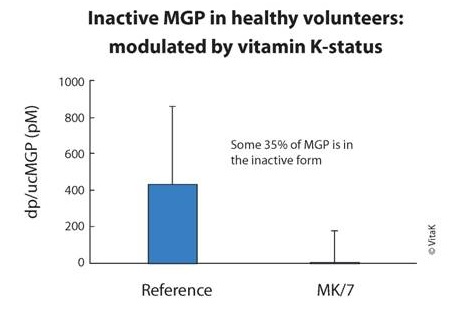
Figure 7: Supplementation with MK-7 results in significantly decreased levels of inactive MGP, resulting in significantly more active MGP. (The dose was 360 mcg of MK7 for three months). Courtesy of Dr. Schurgers.
Passwater: In order to gamma-carboylate MGP, vitamin K itself must cycle between various forms as shown in Figure 8.
Schurgers: The reduced form of vitamin K, vitamin K hydroquinone (vitamin KH2), is the actual cofactor for the gamma-carboxylases as it is converted to vitamin K epoxide. Proteins containing gamma-carboxyglutamate are called Gla proteins. The two vitamin K-dependent proteins found in bone are osteocalcin, also known as bone Gla (gamma-carboxyglutamate) protein or BGP, and the matrix Gla protein or MGP.
Passwater: MGP and osteocalcin are both calcium-binding proteins that may participate in the organization of bone tissue. Several nutrients (including the major minerals calcium and phosphorus) are essential for bone health, but bone tissue is organic, not just mineral. Bone consists of a matrix of protein that holds the minerals together. Vitamin C is needed for collagen cross-linking. Copper, zinc, manganese and boron are needed as co-factors for the enzymes that act in the synthesis or post-translational modification of constituents of bone matrix. Silicon is needed for collagen production and to act as a cross-linking agent to stabilize the glycosaminoglycan network. Vitamin D is needed to produce osteocalcin. Even if you have more than enough calcium, vitamin D and osteocalcin in your blood, bone formation will be greatly impaired without adequate vitamin K to activate the osteocalcin so that it takes the calcium from the blood and puts the calcium into the bone tissues.
What human evidence is there that vitamin K2 helps maintain bone mineral density?
Schurgers: Several clinical intervention trials have been conducted to show the beneficial effect of vitamin K. Whereas vitamin K1 was shown to reduce bone loss by 35%, vitamin K2 could completely prevent the loss of bone strength in postmenopausal women. The effect of vitamin K is via the activation of the vitamin K-dependent bone protein called osteocalcin. As Figure 8 shows, we and others have shown that in the normal population, some 30% of osteocalcin is in the inactive form. Therefore, extra vitamin K is needed to reduce this fraction.
Passwater: Since the bone-forming and mineralization cells called osteoblasts produce osteocalcin and osteocalcin is inactive until activated by vitamin K, is there evidence that vitamin K2 can overcome osteoporosis?
Schurgers: Osteoporosis is a disease in which the bone mineral density is extremely low. Our studies always focused on postmenopausal women, in which the bone loss is accelerated. We wanted to demonstrate that extra vitamin K could reduce this bone loss and prevent women from becoming osteoporotic. Once women are osteoporotic, we would advise them to visit their medical doctors.
Passwater: Who should consider taking vitamin K2 supplements?
Schurgers: Recent scientific data show even a well-balanced diet might not provide sufficient vitamin K to fulfill the body’s needs. Measuring vitamin K-dependent proteins in many apparently healthy subjects showed that people that do not consume vitamin K-supplements have some 30% inactive vitamin K-dependent proteins. As these inactive proteins are correlated with bone and vascular disease, everybody should consider taking some extra vitamin K2. In this way, we can remove this risk factor.
Passwater: What type of vitamin K supplement is best?
Schurgers: Currently, there are three types of vitamin K available as supplements including synthetic vitamin K1, menaquinone-4 (MK-4), a vitamin K2 which is not extracted from a natural food source as (MK-4), and natural vitamin K2 as menaquinone-7 (MK-7) as shown in Figure 9. Due to the deficiency of K vitamins in most people as a result of the Western diet, I recommend supplementation for optimal bone and cardiovascular health. If you have a choice, vitamin K2 is preferable to K1, as K2 intake has been linked to both bone and cardiovascular health. And, as Figure 10 shows, the most desirable form of K2 is natural vitamin K2 as MK-7, as this is the most bioavailable, bioactive and longest lasting form of vitamin K available. Our laboratory has tested one MK-7 product (MenaQ7) for safety and efficacy in humans, and thus I can recommend it.
Passwater: Where does your research take you next?
Schurgers: I am currently preparing and planning three big clinical trials with medical doctors: one trial in aortic stenosis patients (cardiology department), one in dialysis patients (a multicenter trial including some 500 patients) and one trial in cardiac patients with calcifications and hypertension. All trials will be conducted with 360 mcg of MK-7.
Passwater: This will be very important research. I know of a lot of women who would appreciate seeing a study of vitamin K2 versus breast soft-tissue califications. Biochemistry logic suggests that vitamin K2 could reduce breast calcifications and thus, reduce the need for many biopsies.
Thank you ,Dr. Schurgers, for your research and for chatting with us about the importance of vitamin K2 in bone and artery health. I know our readers are looking forward to chatting with you again as more of your research is finished, and, perhaps we can also incude a discussion about the workings of the vitamin K cycle.
Readers can find more information about vitamin K2 at http://vitamink2.org .
This article was originally posted here:
- http://www.drpasswater.com/nutrition_library/Schurgers.html
- http://www.drpasswater.com/nutrition_library/Schurgers2.html
Learn from the Experts:
1) Great interview with Dr. Kate Rheaume-Bleue on Vitamin K2:
2) Dr. John Whitcomb Seminar – Vitamin K2 – Super Vitamin, Hidden Before Our Eyes
The Human Diet Evolution & its Impact on Human Health

The evolution of the human diet over the past 10,000 years from a Paleolithic diet to our current modern pattern of intake has resulted in profound changes, not only in our in feeding behavior, but our overall health.
Shifts have occurred from diets high in fruits, vegetables, lean meats and seafood, to processed foods high in sodium and hydrogenated fats, and low in fiber. These changes have left bodies void of the nutrients that provide the foundation for health, resulting in an increase in obesity and chronic disease.
Paleolithic Diet
Growing Opportunities
Humans began domesticating animals between 4,000 and 10,000 years ago. Managing the whereabouts of docile creatures provided a reliable source of nutrition.
Meanwhile, agriculture was invented around 8000 BC, which allowed humans to control food sources via planting and harvesting. In time they began experimenting with plant species, planting only the choicest specimens and weeding out undesirable characteristics.
This marked the beginning of the end of man’s hunter-gatherer, food-as-survival history.
Manmade Fats
In 1902, scientist Wilhelm Normann found that liquid oils could be hydrogenated to form trans fatty acids. With Proctor & Gamble’s introduction of Crisco vegetable shortening, the first manufactured trans fat product hit grocery store shelves in 1911, leading to trans fat being the first manmade fat to join the food supply.
Chemical Influence
 Natural farming processes, which were developed over 1000s of years, are abandoned for scientific farming processes.In 1910, the first legislation is passed providing federal authority for regulating pesticides. While fertilizers and pesticides allowed for more efficient growing, the former comes at a cost of micronutrient depletion of the soil (i.e., selenium), the latter having toxic effects on the human system.
Natural farming processes, which were developed over 1000s of years, are abandoned for scientific farming processes.In 1910, the first legislation is passed providing federal authority for regulating pesticides. While fertilizers and pesticides allowed for more efficient growing, the former comes at a cost of micronutrient depletion of the soil (i.e., selenium), the latter having toxic effects on the human system.
Nutrient-Depleting Firsts
Feedlot Frenzy
The first cattle feedlots are opened in 1950. The poultry industry began moving chickens off pasture and into buildings later that decade. The dairy industry followed suit in the 1960s, and pork producers in the 1970s.
Removing animals from pasture meant we inadvertently remove vitamin K2 from common dietary staples, such as butter, eggs, cheese and meat, as grass-grazing animals convert vitamin K1 to vitamin K2 (MK-4).
More But Less
 Since 1980, populations have been consuming an extra 300 calories a day, but roughly 92% of them in the form of sugars, fats and mostly refined. By 1990, “natural” is an unrecognizable food characteristic due to the rampant use of Artificial Sweeteners and Flavoring in food and drink, as well as enormous portion sizes.
Since 1980, populations have been consuming an extra 300 calories a day, but roughly 92% of them in the form of sugars, fats and mostly refined. By 1990, “natural” is an unrecognizable food characteristic due to the rampant use of Artificial Sweeteners and Flavoring in food and drink, as well as enormous portion sizes.
Chemical Consequences
 The 1990s also saw an increased use of hormones and steroids in cattle feed, while the new millennia saw that 80% of antibiotics in the U.S. are found in food, with 28.9 million pounds going to livestock. (But humans weren’t left out: they received a staggering 7.3 million pounds of antibiotics.)Overuse of antibiotics has led to more antibiotic-resistant bacteria, which has depleted the body of the good bacteria in the gut. Not only has this led to intestinal discomfort and weakened immune systems, but it has also directly contributed to the obesity epidemic.
The 1990s also saw an increased use of hormones and steroids in cattle feed, while the new millennia saw that 80% of antibiotics in the U.S. are found in food, with 28.9 million pounds going to livestock. (But humans weren’t left out: they received a staggering 7.3 million pounds of antibiotics.)Overuse of antibiotics has led to more antibiotic-resistant bacteria, which has depleted the body of the good bacteria in the gut. Not only has this led to intestinal discomfort and weakened immune systems, but it has also directly contributed to the obesity epidemic.
Weighty Worries
 Today, more than one-third of the U.S. adults are considered obese. Worldwide, obesity has nearly doubled since 1980.More alarming: By 1989, children’s diets show major deficiencies in minerals and key vitamins, such as iron and vitamin K. Factors such as these have contributed to more than 40 million children under the age of 5 being overweight in 2011.
Today, more than one-third of the U.S. adults are considered obese. Worldwide, obesity has nearly doubled since 1980.More alarming: By 1989, children’s diets show major deficiencies in minerals and key vitamins, such as iron and vitamin K. Factors such as these have contributed to more than 40 million children under the age of 5 being overweight in 2011.
The Verdict
 Since abandoning natural farming process, the human diet has changed dramatically. These changes have run in parallel with changes in lifestyle and disease patterns. Poor nutrition creates major problems for the young as they grow older, particularly in terms of chronic disease patterns related to a breaking down of the immune system. Dietary intakes have implications for the health of the bone and the cardiovascular systems in later adulthood.The evolution of our diet may provide answers to the emergence of modern disease, just as the correction of (or supplementation to) our modern diets could hold the key to treating or preventing many of these chronic conditions.
Since abandoning natural farming process, the human diet has changed dramatically. These changes have run in parallel with changes in lifestyle and disease patterns. Poor nutrition creates major problems for the young as they grow older, particularly in terms of chronic disease patterns related to a breaking down of the immune system. Dietary intakes have implications for the health of the bone and the cardiovascular systems in later adulthood.The evolution of our diet may provide answers to the emergence of modern disease, just as the correction of (or supplementation to) our modern diets could hold the key to treating or preventing many of these chronic conditions.
Testing for Vitamin D
Having blood tests to measure the amount of vitamin D in your blood is the only way to know if you’re getting enough vitamin D or not. The blood test you need is called a 25(OH)D blood test.
You can get a blood test at your doctors or you can do an in-home test or get a test at a laboratory. All of these methods of testing should give you accurate results.
In-home tests are easy to use and involve pricking your finger to take a small blood sample and sending this away to a laboratory for testing.
Your tests results will show whether you’re getting enough vitamin D or not, and whether you may need to take supplements or expose your skin to the sun more. Different organizations in the United States recommend different ideal vitamin D levels. The Vitamin D Council suggests that a level of 50 ng/ml is the ideal level to aim for.
How do I get tested?
There are three ways to get tested:
- Ask your doctor for a vitamin D test. Be specific and ask for a 25(OH)D test. There is another type of blood test for vitamin D, called a 1,25(OH)₂D test, but the 25(OH)D test is the only one that will tell you whether you’re getting enough vitamin D. If your health insurance covers a 25(OH)D test, this is a good way to work with your doctor to get tested.
- Order an in-home test. These tests are sent to your home. You prick your finger and put a drop of blood on to some blotter paper. You send the paper to a laboratory to be tested. These are an alternative if you don’t want to go to your doctor just for a vitamin D test, or if your insurance doesn’t cover a test.
- Order a test online and get blood work done at a laboratory. In the United States, there are a few websites that allow you to bypass your doctor and go straight to the testing laboratory. These websites include mymedlab.com, healthcheckusa.com and privatemdlabs.com. You can buy a 25(OH)D test from all of these companies and have the test itself done at your nearest LabCorp. These tests are a little more expensive than in-home tests.
All three ways of getting tested should give you an accurate result.
Where can I get an in-home test?
There are a number of companies that offer in-home tests, including:
- Vitamin D Council. The Vitamin D Council has recently released it’s own in-home vitamin D test kit. Partnering with Heartland Assays, the Council is bringing the most affordable home testing solution available in the United States.
- ZRT Labs. The Vitamin D Council works with ZRT Labs and receives 15% of the proceeds from each test bought. This helps to support the Vitamin D Council (a nonprofit organization!) and gives you accurate test results.
- New Century Diagnostics. The test is sold through a website called Home Health Testing. Some users report that the test is a little difficult to use.
- City Assays. This company is based in the UK and offers the cheapest test internationally (about $48 USD) and in the UK/Ireland (£25). It takes about 10 days for the test to arrive to the United States.
To the Vitamin D Council’s knowledge, all of these in-home tests are accurate.
What do the results mean?
When you get your test results you will see a number in units of ng/ml, for example, 50 ng/ml. These are the units that health professionals in the United States use. Elsewhere in the world, vitamin D blood test results are given in units of nmol/l.
To convert a test result measured in nmol/l to one measured in ng/ml, divide the nmol/l number by 2.5. For example, 50 nmol/l is the same as 20 ng/ml (50÷2.5).
To convert a test result measured in ng/ml to one measured in nmol/l, multiply the ng/ml number by 2.5. For example, 20 ng/ml is the same as 50 nmol/l (20 x 2.5).
These are the ranges that different organizations in the United States use to say whether you’re severely lacking in vitamin D (deficient), mildly lacking in vitamin D (insufficient) or whether you’re getting enough vitamin D (sufficient):
| Vitamin D Council | Endocrine Society | Testing Laboratories | ||
| Deficient | 0-30 ng/ml | 0-30 ng/ml | 0-31 ng/ml | |
| Insufficient | 31-89 ng/ml | 31-79 ng/ml | 32-89 ng /ml | |
| Sufficient | 90-120 ng/ml | 80-120 ng/ml | 90-120 ng/ml | |
| Toxic | >150 ng/ml |
The Vitamin D Council suggests that a level of 110 ng/ml is the ideal level to aim for. This is why the Council recommends that adults take 10,000 IU/day of vitamin D supplement in order to reach and stay at this level.
The Endocrine Society recommends taking a vitamin D supplement of around 10,000 IU/day to reach and stay above a level of 80 ng/ml. This is what the Endocrine Society recommends as the ideal level to aim for.
What should you do based on your test results?
- If you tested low and want a higher level, you need to get more sun exposure or take a larger daily supplement.
- If you tested and are right where you want to be, continue your supplement and sun exposure routine. Keep in mind that your level in the summer is probably higher than in the winter, with more sun and UVB. So you may need to supplement more in the winter than in the summer to have the same vitamin D level.
- If you tested high and want a lower level, you need to take a smaller daily supplement.
You do not want to have a level over 150 ng/ml and (in fact anything over 150 ng/ml is considered toxic.)
References
- Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM; Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011 Jul;96(7):1911-30.
- Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: National Academy Press, 2010.
- Vieth, R. “The Pharmacology of Vitamin D.” In Vitamin D, Third Edition, by Feldman D, Pike JW and Adams JS. Elsevier Academic Press, 2011.
Where to Buy:
- Vitamin K2 (in MK-9 form) 500mcg x 1000 tablets for £7.86 + £36.99 Shipping = £44.85 = US$72.72
- Vitamin D3 (10,000 IU) x 360 Softgels for US$19.70 + FREE Shipping
—> Coupon for 15% off at pureformulas.com: WLCBEJN115
Action Step / Dosage:
Remember Vitamin D3 & Vitamin K2 need to be taken together — the recommended ratio is:
For every 1000 IU of D3, take 100-200mcg of K2 (in the form of MK-7 or higher [MK-9])
I like to get their Vitamind D3 blood levels up to about 100-120 ng/ml. For many people that takes from 10,000 IU (up to 20,000 IU) of vitamin D3 daily. The best way to determine if your blood levels are high enough is to get your blood tested.
For Daily Usage:
If taking 10,000 IU of Vitamin D3 —-> |
take 1,000 to 2,000 mcg of Vitamin K2 (in form of MK-7 or higher [MK-9]) |
If taking 20,000 IU of Vitamin D3 —-> |
take 2,000 to 4,000 mcg of Vitamin K2 (in form of MK-7 or higher [MK-9]) |






Discussion
Trackbacks/Pingbacks
Pingback: All About Juicing (vegetables) | Make Better Habits - June 17, 2015