The last ten years has seen a huge body of research evidence showing that:
- Vitamin D is an important factor in cancer prevention.
- Vitamin D activates the immune system to work against rogue cells.
- Vitamin D has the ability to normalize and correct cancer cells – it is the ´ultimate epigenetic compound´.
So, it boosts the immune system, prevents cancer, AND (according to several research studies) may even help beat it.
2015 research shows that its levels in your blood at the time of diagnosis can also predict survival times in breast cancer.
Researchers from University of California, San Diego analyzed five past studies of breast cancer patients, accounting for 4,443 people. Women with a greater chance of surviving breast cancer had an average vitamin D level of 30 nanograms per milliliter, while the women who had less chance of surviving had an average of 17 nano grams per milliliter.
Unfortunately, most newly diagnosed breast cancer patients are at the deficient end of the spectrum.
In fact, women with high levels of vitamin D were more than twice as likely to survive breast cancer than women with low levels of vitamin D. (Study published in the Journal of Anticancer Research)
And vitamin D has been shown effective at controlling low grade prostate cancers after diagnosis, without the need for orthodox treatment.
´Vitamin D supplements could slow or even reverse the progression of less aggressive, or low-grade, prostate tumors without the need for surgery or radiation´. That is according to new research on the subject. However the researchers report that higher doses of vitamin D could have significant benefits with more advance prostate cancer, but this was outside the scope of their study and nothing is confirmed as yet.
The research came from a team at the University of Southern Carolina and was reported at the 249th National Meeting & Exposition of the American Chemical Society (ACS), March 22nd 2015.
If a tumor is present in a prostate biopsy, a pathologist grades its aggressiveness on a scale known as the Gleason Grading System. Tumors with Gleason scores of 7 and above are considered aggressive and likely to spread, requiring surgical removal of the prostate gland (prostatectomy) or radiation therapy. In contrast, prostate tumors with Gleason scores of 6 and below are less aggressive, and in some cases may cause no symptoms or health problems for the duration of the man’s life.
“In cases of low-grade prostate cancer, many urologists do not treat the disease, but instead do what’s called ´active surveillance´,” says Bruce Hollis, Ph.D., who is at the Medical University of South Carolina.“The cure — meaning surgery or radiation — is probably worse than the disease, so they wait a year and then do another biopsy to see where the patient stands.”
However, knowing that they have even low-grade prostate cancer can cause patients and their families excessive anxiety, which prompts some of the men to undergo an elective prostatectomy, despite the risk of complications such as infection, urinary incontinence and erectile dysfunction. But a man must wait 60 days from the time of his biopsy before he can undergo a prostatectomy, so that inflammation from the biopsy can subside.
Hollis wondered if giving these men vitamin D supplements during the 60-day waiting period would affect their prostate cancer. His previous research had shown that when men with low-grade prostate cancer took vitamin D supplements for a year, 55 percent of them showed decreased Gleason scores or even complete disappearance of their tumors compared to their biopsies a year before (J. Clin. Endocrinol. Metab., 2012, DOI: 10.1210/jc.2012-1451).
In a new randomized, controlled clinical trial, his team assigned 37 men undergoing elective prostatectomies either to a group that received 4,000 U of vitamin D per day, or to a placebo group that didn’t receive vitamin D. The men’s prostate glands were removed and examined 60 days later.
Preliminary results from this study indicate that many of the men who received vitamin D showed improvements in their prostate tumors, whereas the tumors in the placebo group either stayed the same or got worse. Also, vitamin D caused dramatic changes in the expression levels of many cell lipids and proteins, particularly those involved in inflammation. “Cancer is associated with inflammation, especially in the prostate gland,” says Hollis. “Vitamin D is really fighting this inflammation within the gland.”
The protein most strongly induced by vitamin D was one called growth differentiation factor 15 (GDF15). Previous studies by other groups showed that GDF15 dials down inflammation, and many aggressive prostate cancers make little or no GDF15.
The new research suggests that vitamin D supplementation may improve low-grade prostate cancers by reducing inflammation, perhaps lessening the need for eventual surgery or radiation treatment.
“We don’t know yet whether vitamin D treats or prevents prostate cancer,” says Hollis. “At the minimum, what it may do is keep lower-grade prostate cancers from going ballistic.”
Hollis notes that the dosage of vitamin D administered in the study — 4,000 IUs — is well below the 10,000–20,000 IUs that the human body can make from daily sun exposure. “We’re treating these guys with normal body levels of vitamin D,” he says. “We haven’t even moved into the pharmacological levels yet.”
All of which really does make a nonsense of health bodies and cancer charities who tell you to stay out of the sun because you might get skin cancer! In 2014 vitamin D was shown to make certain chemo drugs work better,
Researchers have shown that vitamin D given in conjunction with gemcitabine chemotherapy in mice results in a 57% increase in survival over chemo on its own.
29% of the mice were considered ‘long-term survivors. Pancreatic cancer cells were shown to have vitamin D receptors. Human clinical trials are now underway. Dr Ronald Evans, who directs the Salk Gene Expression Laboratory in La Jolla, California lead the research covered in the journal Cell.
“These (PCS) cells basically recognize the cancer as a big wound and they surround the tumor, become activated, and start excreting a lot of extracellular matrix that acts like cement,” explained study researcherMichael Downes, PhD, of the Salk Institute.
“This is one reason pancreatic cancer is so hard to treat. It is difficult to get chemotherapy drugs to the tumor because this ´wound´ has been walled up by these cells,” he told MedPage Today. “The vitamin D analog tears down this wall to some extent so the chemotherapy drugs can get in.”
“For pancreatic cancer, the five-year survival rate is the lowest of all cancers,” says Evans, holder of Salk’s March of Dimes Chair and a Howard Hughes Medical Institute investigator. “Part of the problem is that the science of pancreatic cancer and its renowned resistance to therapy has not been understood and that’s why the work that we’re doing is so important.”
ED: We have been telling you about the benefits of vitamin D for years. Like Harvard Medical School, we believe everybody with cancer should take 5,000 IUs a day, if they cannot go in the sun for 4 hours.
But, yet again, here is research (albeit not in humans) that shows some supplements are capable of IMPROVING orthodox medicine. Too many oncologists tell their patients to refrain from taking any supplements while on Chemotherapy – and they are wrong to do this.
Reference: Vitamin D Receptor-Mediated Stromal Reprogramming Suppresses Pancreatitis and Enhances Pancreatic Cancer Therapy (http://www.cell.com/abstract/S0092-8674(14)01033-2)
Researchers in America are proposing to use it as part of a hormone therapy package with breast cancer patients.
Dr. Tan Ince is a pathology professor at the University of Miami and an accomplished breast cancer researcher He is working on a new personalized multi-hormone treatment protocol for breast cancer patients.
 And one of the hormones he is looking at is … vitamin D. As we have told you before – it’s not really a vitamin, it’s a hormone!
And one of the hormones he is looking at is … vitamin D. As we have told you before – it’s not really a vitamin, it’s a hormone!
As a member of the Sylvester Comprehensive Cancer Center, Ince has spent the past 15 years researching the role of non-genetic factors in the development of cancer.
In a peer-reviewed paper published in 2014, Ince’s research identified at least 11 distinct breast cell ‘subtypes’, going on to determine that each of these subtypes have hormone receptors that all behave uniquely — and have the potential to respond to oestrogen, Vitamin D and androgen (or to just one or two of these hormones).
“This was the first time any breast-cancer research had been done on all three hormones simultaneously,” Ince says. Ince’s thesis is that doses of chemotherapy can be reduced by using combinations of two of the three, and he is hoping to go to clinical trials soon.
Professor Hollick of Harvard Medical School once proclaimed that “25% less women would die of breast cancer if they had adequate levels of vitamin D in their blood”.
You can really only derive vitamin D from sunshine on the skin, or supplementation. A little comes from fish oils. Harvard recommended that every cancer patient took 5,000IUs a day (that´s about 4 hours in good sunshine)
Oh, and if that´s not enough, it seems to play an important role in preventing all manner of illnesses too!
For example:
- low levels of vitamin D have been linked to an increased risk of Alzheimer´s and dementia (click here).
- Low levels of vitamin D linked to type-2 diabetes risk (click here).
- Low levels of vitamin D linked to MS (click here).
Vitamin D – are you getting enough?
Harvard Medical School has conducted a large amount of research on vitamin D. Firstly, as you will see, it acts like a hormone rather than a vitamin. Secondly virtually everyone with cancer (yes even those with melanoma) seem to be deficient in vitamin D. Harvard suggest everyone with cancer should take 5,000 IUs a day – that´s 4 hours in good sunshine, or supplementation. It is only in very low levels in food.
Research shows it has many varied capabilities, for example:
- Research in 2012 in Cancer Causes and Control presented findings that former/never smokers were 44 per cent less likely to die fromlung cancer if they had blood levels of vitamin D above 44 nmo/litre. That applied to whether or not they had the cancer – it seems to prevent, and reduce deaths.
- In 2013, researchers from St Louis University showed that women with a BRCA1 mutation are more likely to develop an aggressivebreast cancer but vitamin D can block this pathway. BRCA1 is not just behind breast cancer but other cancers too like some prostate cancer. Clinical trials are now planned.
- Another 2013 study, this time in the Journal of Cellular Biology showed that vitamin D blocks cathapsin L which makes cells grow uncontrollably in cancers.
In fact, Vitamin D has epigenetic benefits. Rarely is the DNA code actually mutated. What happens most usually in cancer is that the chemical bonds around the DNA change (due to poor diet, environmental toxins, stress and so on). When the bonds change, certain genes get blocked – they can´t express themselves. They are silenced. If it was a tumour suppressor gene then you can see the problem. But Scientists now know that these changes are reversible. They are looking for drugs to do the job. But natural compounds like vitamin D, curcumin, fish oils, CLA, sulphorapanes are also capable of making these changes. Thus vitamin D both protects AND corrects.
The vitamin that works like a hormone
Vitamin D may sound like a vitamin, but it acts more like a hormone with receptor sites on healthy cells and even more on cancer cells. Researchers at the University of Miami Medical School are using it as a part of their hormone therapy for breast cancer. Let´s look at three of the areas in which it acts:
-
Low vitamin D levels are linked with higher rates of cancer
For example: Vitamin D and breast cancer – The Boston University School of Medicine has completed a great many research studies on vitamin D. Read the following statement from their Professor Michael F. Holick, “If women obtained adequate levels of vitamin D there would be 25 per cent less deaths from breast cancer.
Holick is not alone in stressing the importance for women and breast cancer. St Georges Hospital in London calculated from their studies that women with low levels of vitamin D in their breast tissue have a 354 per cent greater risk of breast cancer. Translated into English this means they have 4 and a half times the breast cancer risk. You can read more from Holick HERE.
-
Immune booster
As you will see below, when it comes to fighting cancer, there seems little doubt about the virtues of this vitamin. Indeed many experts believe it is more like a hormone having receptor sites on both the cell and nuclear membranes – especially in cancer cells! According to research from the University of Copenhagen in 2010, when T-lymphocytes of the immune system come across a pathogen, the first thing they do is bind to a vitamin D molecule to ´activate´ themselves.
Recent studies covered in Cancer Watch suggest that the action of vitamin D is enhanced by vitamin K. Most adults are increasingly short of both D and K vitamins.
2012 research from the University of Carolina showed that children with low blood levels of vitamin D were more likely to become critically ill.
-
A Natural Cancer ´Cure´?
Research published in the Journal of Cell Biology November 17, 2008; 183(4):697-710 has shown that “vitamin D can adjust almost everything in the cancer cell, from its genetic messaging to its cytoskeleton. It can switch genes on and off, and it can reduce cell division, and it can calm the cancer cells so that they settle rather than spread. It seems vitamin D can actually return a cancer cell to a normal and healthy state. One pathway seems to control everything”. That is a very important set of findings. And there are many more studies on its corrective epigenetic benefits.
-
It makes some drugs work better
Researchers at the Salk Institute have shown that the pancreatic cancer drug gemcitabine works 57 per cent better if combined with vitamin D.
If you are in any doubt about its potential, then the pharmaceutical companies are certainly not. For example, Memorial Sloan-Kettering were involved in a Phase III clinical trial where a synthetically made, concentrated form of vitamin D, called Asentar, significantly improved patient survival times. “It has enormous potential”, said Dr Howard Scher, team leader. Unfortunately, politics took their toll on the trial – but that´s another story.
At CANCERactive we are very clear about vitamin D. There is more than enough research to be clear that vitamin D can help prevent cancer. And, from the latest studies, it is increasingly clear that every cancer patient should be having a daily half hour in the sunshine, or supplementing.
The question is …
When it comes to vitamin D, are you getting enough?
The sunshine factor
So alarmed are we by other cancer charities and cancer bodies continually delivering the message that somehow sunshine is bad for you, that we launched the CANCERactive SAFESUN campaign to tell people the truth, without politics or vested interest, on how to make the most of sunshine for good health.
´Practise SafeSun´
The CANCERactive Campaign to get more from your sunshine!
1) Try to get at least 30 minutes in the sunshine every day of your life. It is essential to your good health, your immune system and cancer prevention.
2) However, do not go from the dark British Winter and immediately spend the first days of your holiday under a mid-day tropical or mountain sun. Build up tanning slowly, using early mornings or late afternoons – it takes about 4 days to activate your pigmentation; before that you are in danger of tissue damage.
3) Do not burn. Be sensible. Be safe.
4) Be aware of your own skin type.
5) Avoid all sun screens, lotions, aftersun creams and skin creams/moisturisers that contain PABA, parabens, retinyl palmitate, retinol palmitate and oxybenzone, or come in plastic bottles you are unsure whether or not they have BPA or Phthalates from their plasticisers. Never leave your plastic bottle directly in the sun. (To read more on this click here)
6) As an ´aftersun´, use pure Aloe Vera gel to help repair any damage.
7) Always wear sunglases and consider a hat.
8) Be wary of sunbeds and artificial tanning lights. There has been research expressing concerns and official warnings.
9) If you are taking HRT or an oestrogen-based contraceptive pill, be even more cautious than others. The oestrogen may pre-sensitise your skin.
10) Sunshine´s action on your skin makes essential vitamin D in your body. If you cannot go in the sun, and are living a predominantly indoor city life, supplement with 5000 IUs of vitamin D per day. (Click this link to read ´Vitamin D – Are you getting enough?´ our report on the vitamin that is essential to your good health – and to beating cancer).
********************
i) Other things to consider from research are boosting your diet in advance, with oily fish, carotenoids (like carrots, red and yellow peppers and watermelon), flavenoids including resveratrol (grape skins, red wine), and olive oil; and going in the sea in preference to chlorinated swimming pools.
ii) 2011 research shows that a combination of vitamin D and calcium (one helping of ´greens´ per day) significantly reduce skin cancer risk.
But doesn´t sunshine cause skin cancer, and even melanoma?
Up front I would point out that there are several studies which show over 90 per cent of people with melanoma are deficient in vitamin D;and others which show that people who have regular exposure to sunshine develop LESS cancers! Furthermore, 2011 research showed half of melanoma is found in locations not exposed to the sun.
Vitamin that cuts risk of cancer
Two studies had been presented in the USA and both showed that women with the highest levels of vitamin D were up to 50 per cent less likely to develop breast cancer. One study involved St. Georges Hospital Medical School in London and US researchers at Harvard and University of California; the other was carried out by Canadian researchers at Mount Sinai Hospital in Toronto. Both were presented at a meeting of the American Association for Cancer Research in Washington. The doctors in the research concluded, Women with high exposure to the sun as teenagers may be protected against breast cancer in later life, and Boosting levels of vitamin D could be beneficial at a time when breast cells are developing. So much for the charities who have been warning us against sun exposure!
New research on Cancer Prevention is coming thick and fast:
- Moores Cancer Centre at UCSD, San Diego concluded from a mega study of previous research that up to half the cases of breast cancer, and two thirds of the cases of colorectal cancer in the USA could have been prevented if people had had adequate blood levels of vitamin D.
– The Journal of Steroid Biochemistry and Molecular Biology reviewed two studies concluding that women with the highest blood levels had the lowest risk of breast cancer 15 to 30 minutes in the sun every day, or 2000 IUs of supplement were recommended. One study showed that the lower blood levels of vitamin D, the more dense (and dangerous) the breast tissue.
– The American Journal of Preventative medicine cross-related 5 studies over a 25 year period to conclude that taking a 2000 IU supplement of vitamin D3 daily would cut colorectal cancer by two thirds.
- Science Daily (Sept 12 2006) covers two large scale research projects of 125,000 men and women, concluding that just 400IUs could reduce pancreatic cancer risk by 86 per cent.
- A UK study covering 1.1 million men and women concluded that higher levels of blood vitamin D meant fewer deaths from cancer.
- In the Journal of Clinical Oncology (Jan 20, 2005) men with the highest levels of vitamin D in their blood were half as likely to develop prostate cancer, as those with poor amounts. Research has shown that vitamin D inhibits prostate cancer cell growth. The provider of the vitamin in the research? Sunshine!
- St Georges Hospital showed that the provision of 400IUs of vitamin D reduced pancreatic cancer by 34 per cent.
- Sunshine reduces risk of Hodgkins by 40 per cent (Karolinska Institute).
But what if you already have cancer?
As we reported in the introduction research published in the Journal of Cell Biology November 17, 2008; 183(4):697-710 has shown that vitamin D can adjust almost everything in the cancer cell and return it to the normal, healthy state. Another study has shown that vitamin D can bind to mutated cancer cell receptor sites and cause cell death.
But theres more. For example:
- Researchers at the Harvard Medical School and Harvard School of Public Health have concluded that good levels of vitamin D in the body may help people with early stage lung cancer survive longer after surgery. Patients who had surgery in the sunny summer months where vitamin D levels are higher were more than twice as likely to be alive 5 years after surgery compared with those with low vitamin D levels having winter time surgery.
Dr David Christiani said the survival differences were dramatic; the highest levels of vitamin D saw 72 per cent 5- year survivals compared with just 29 per cent for people with the lowest levels.
It looks like vitamin D is antiproliferative, as it inhibits proliferation of abnormal cells, added Christiani, and there was also evidence to suggest vitamin D inhibits the spread of tumours.
- A study reported in September Cancer Watch 2008, led by Pamela Goodwin, MD, Professor of Medicine at the University of Toronto, research concluded that women with vitamin D deficiency at the time of breast cancer diagnosis were 94 per cent more likely to experience cancer spread and 73 per cent more likely to die over the next 10 years compared to women with adequate vitamin D levels.
- Breast cancer cells have been shown to have vitamin D receptor sites on their surface. Since women who have had breast cancer in one breast are clearly interested in preventing breast cancer in the other, supplementation of vitamin D seems an essential part of their anti-cancer programme.
And vitamin D supplementation is already being used as part of breast cancer treatment programmes in some US hospitals; it is being used in conjunction with radiotherapy in others, and it is also being used in a concentrated form in combination with Taxotere, for patients with prostate cancer at Memorial Sloan-Kettering New York.
If you cant get in the sun every day and you want to obtain vitamin D supplements, Natural Selection has an all natural, product of choice vitamin D3 which you can access by clicking this link.
Essential
What is becoming clear in all the recent scientific studies on vitamin D is that:
- A deficiency plays a crucial role in increased risk of cancer and a number of other illnesses
- Most people in our modern Western world are deficient. This is hardly surprising as they may live in colder, rainer climates with little winter sun; they may live out of the sun – watching TV indoors and working in offices; they may even refrain from enjoying sunshine because several major charities have ridiculously warned them against sunshine!
- You can only obtain reasonable quantities of this vitamin through exposure to sunshine; a far lesser amount may be obtained through consuming oily fish. After that, other foods contribute very little. So the third option is supplementation; take your pick!
First Discoveries
Lets go back to the beginning. In 1919 Sir Edward Mellanby was working indoors with dogs and horses during the winter and concluded that if they didnt get sunlight they developed bone disorders. He further concluded that the essential action of fats preventing these problems was due to a vitamin; and that cod liver oil was a strong preventative agent (see also icon articles on fish oils: click here).
The chemical structure of this vitamin, which he named factor X, was identified in the 1930s by Professor A Windaus. And thus vitamin D came about. Bone disorders had also been noted in humans – typically rickets in children.
The Vitamin That Acts Like A Hormone
As we shall see, it is now known that this substance is not technically a vitamin at all, but acts as a classic steroid hormone! The definition of a hormone is that it has DNA receptor sites on the nucleus inside cells, so able to control the “expression” of DNA to build molecules. Vitamin D is an essential part of the endocrine system as it controls the growth and differentiation of cells, the synthesis of key enzymes, several of the adrenal hormones and appears to have other direct DNA functions and even be involved in DNA repair. Recent research has shown completely new and crucial functions: Vitamin D is now known to also have a significant effect on nuclear receptor sites, as well as having receptor sites on cell membranes, and increased numbers on cancer cell membranes.
The Biochemistry of Vitamin D
Vitamin D is an umbrella term for a number of fat-soluble chemicals called calciferols. Vitamin D2, ergocalciferol, is produced when ergosterol in a yeast extract is converted by the ultraviolet component of sunlight. It is never naturally present in human blood, whereas vitamin D3, cholecalciferol, is produced by the same action of UV light on 7-dehydro-cholesterol, a precursor molecule of cholesterol present in our skin. If this does not happen, 7-DHC is converted into cholesterol instead, and then into the other steroid hormones.
Vitamin D3, once manufactured or ingested, is converted first into the 25-hydroxy-cholecalciferol – or 25(OH)D3 – form in the liver, then into 1,25-dihydroxy form – 1,25(OH)2 D3 – in the kidney. It was thought that only the final, 1,25(OH)2D3 form had any activity, but its now clear, firstly, that the 25(OH)D3 form does have effects on cell metabolism, and secondly that several other forms are produced in the skin in lesser quantities that may also have their uses. 70 years after it was first described, our knowledge of vitamin D is developing with increasing speed.
Only recently, tissues other than the kidney have also been found to turn calcidiol into calcitriol and now this is known to help regulate localised, cellular gene expression.
This may be autocrine (inside the cell) and/or paracrine (surrounding the cell). These autocrine and paracrine functions are significantly diminished in vitamin D deficient people. Several studies show many Americans – up to 90 per cent and especially black Americans – are vitamin D deficient, and this is being linked to, for example, a threefold higher level of prostate cancer in black US city dwellers, over their white counterparts.
All this is a long way beyond those first views of vitamin D, where deficiencies were only associated with rickets in the young and osteomalacia in adults.
Vitamin D And Bones
Vitamin D is essential for maintaining bone density and preventing osteoporosis as it helps the absorption of the bone-building materials calcium and phosphorus. In this action it is helped by magnesium.
Vitamin D and cortisol (the stress hormone) have recently been shown in the USA to be the crucial determinants in osteoporosis. Not oestrogen.
Cortisol can bind with receptor sites on bone cells normally used for natural progesterone (not natural oestrogen) and this weakens bone structure. Apart from taking HRT many doctors will advice more dairy. Dairy foods provide high levels of blood calcium (and a tiny amount of vitamin D). However this calcium surge actually depresses vitamin D levels and the bodys ability to absorb magnesium. Catch 22. Dairy gives you high blood calcium, but low bone calcium.
Much work has been done on the effect of vitamin D with bones. For example, in 1991 Tufts University, Boston showed that vitamin D was essential for improving bone density and supplementation was important in the winter months. This work was confirmed in Lyon, France (a thousand miles south of the UK!) in 1992 where a group taking 800 IUs of vitamin D and 1.2 gms of calcium per day had 43 per cent fewer hip fractures and 32 per cent fewer other, non-vertebral fractures. So for osteoporosis think vitamin D and a healthy intake of greens, rather than dairy and HRT supplements!
Sources of Vitamin D
Sunlight on our skin is now thought to be the main source of vitamin D. Night shift workers have lowered blood levels of vitamin D. Heavily tanned, or black people have real problems making vitamin D through the effect of sunlight in their skin. On the other hand, people with Celtic, or Type I skin (ginger hair/ freckles/ burn easily but dont tan), could be said to have skin designed to pick up on any stray bit of UV light in their northerly natural habitat. These days, though, they do tend to avoid the sun, for good reasons, but this can land them with a vitamin D shortage.
Whilst a little is found in dairy foods, the major food source is fish liver oils (omega-3 fish oil supplements dont contain much, though). Cod liver oil is unfortunately a poor source of vitamin D compared to halibut liver oil, while most of the top brands actually contain an added D supplement. Unfortunately, in order to get a useful dose of vitamin D from fish liver oil, you would simultaneously be getting an even bigger dose of vitamin A, which then can interfere with the beneficial effect of vitamin D on bone density – catch 22. (Really this is a biological, practical system of checks and balances. But its thrown out of balance by our near-universal vitamin D deficiency).
Kidney or liver disease (and alcohol) depress vitamin D levels; indeed anything that interferes with the digestion and absorption of oils and fats will – including any form of diarrhoea, diseases such as coeliac and Crohns, and pale bowel motions for whatever reason.
So also do antacids and acid-inhibitors like Zantac, cholesterol-lowering drugs (e.g. statins), mineral oils, anticonvulsants and toxic chemicals in the environment (e.g. smog). Cadmium blocks vitamin D production whilst pantothenic acid helps make it.
Recommended Daily Allowance
So are you getting enough?
Believe it or not, but the current RDA stems from the work of the eccentric Scottish Lord some 80 years ago, and the RDA was set at 5 to 10 micrograms (about 200 IUs) per day over 50 years ago.
However, Dawson-Hughes (Am J Clin Nut 1995; 61) has shown that at that level it has no effect on bone status at all.
Reinhold Veith PhD, University of Toronto, has concluded adults need 5 times this level (Am J Clin Nut May 1999), if they are to maintain healthy bones and, when it comes to cancer, the various research levels use at least 400 IUs daily as a preventative agent.Recommended daily supplementation is 5,000 IUs.
But can high doses cause harm. The answer seems an unequivocal, NO!
On a sunny summer day, a young adult exposing a fair amount of skin for 15-30 minutes will manufacture about 20,000 IUs of vitamin D; this goes down with age to 10,000 IUs or less. This makes a bit of a mockery of the official toxicity safety limit for supplementation of 2,000 IUs.
Veith proposed a level of 4,000 – 10,000 IUs per day for people with cancer and argued that toxicity doesnt start until about 40,000 IUs (Am J Clin Nut 1999; 69). And Harvard Medical researchers totally agree with him.
William B Grant PhD, a vitamin D expert in the USA, believes that 80-90% of Americans are actually deficient in vitamin D. Vitamin D is commercially available as vitamin D2, (ergocalciferol – from plant products, although plants contain very low levels of the vitamin), and vitamin D3, (cholecalciferol – from animal products). The best supplementation to take is vitamin D3. D3 provides vitamin D in its most usable form.
Certainly most anticancer experts suggest people with cancer ensure that they are getting at least 2500 IUs a day, and ideally 5,000 IUs.
Anything Else?
In Cancer Watch November 2010 we covered research from the National Institute for Health in Finland who linked lower levels of blood vitamin D to dementia and Parkinson´s disease.
In icon 2007, issue 2, we reported that researchers in Auckland New Zealand reported that people with higher levels of vitamin D in their blood had lower blood pressure, and vice versa.
In icon Issue Winter 2007/8, we reported that researchers at Kings College London reported that people with higher blood levels of vitamin D aged more slowly.
We are finding out new, and often amazing, things about vitamin D all the time – not so amazing, though, when you remember that it is actually a hormone; the hormone we all forgot about.
Research concludes it may:
- benefit fertility problems by helping the fertilised egg to implant in the womb.
- help the body assimilate vitamin A and have a synergistic effect with both A and E.
- be crucial to the growth, maturation and normal functioning of the immune system.
- be important in both the prevention and the treatment of auto-immune diseases such as rheumatoid arthritis, multiple sclerosis and Type I (insulin-dependent) diabetes. In cases of vitamin D deficiency the body loses its ability to fully produce insulin.
- strengthen muscles as well as bones, improving athletic performance not only in the elderly but probably even in young athletes.
- have anti-inflammatory properties useful not only in diseases such as arthritis but probably even in arteriosclerosis and heart disease.
- help the body to produce natural antibiotic substances
- help to control obesity by, together with calcium, reducing overeating, and boosting fat metabolism. (Overweight is of course a risk factor for both cancer and heart disease).
- help prevent Parkinsons (Emory University, Archives of Neurology)
- it is even reported to help to slow down hair loss!
More on Vitamin D and Cancer
As we said above the new excitement is the discovery that cells contain large numbers of receptor sites for vitamin D.
Vitamin D plays multiple roles in the regulation of animals metabolism; Boston University School of Medicine (Rahul Ray) showed that it has a regulatory effect on plasma membranes affecting all sorts of carried hormones and chemicals, and also on gene transcription. They have conducted much work on these vitamin D Nuclear Receptors (VDRs). Vitamin D is bound in plasma and on nuclear sites and is very much part of the endocrine system.
Epidemology studies have argued that the levels of sunlight and cancer are inversely proportional.Studzinski and Moore (Cancer Research 1995; 55) talked about a belt through America where there was less sunshine and 2-3 times higher rates of cancer.
But where cancer researchers were really turned on was in the finding that vitamin D can regulate cell differentiation and proliferation and even DNA repair mechanisms.
For example, laboratory tests have shown that vitamin D inhibits the growth of the new blood vessels (angiogenesis) needed by tumours in order to satisfy their high metabolism (Shokravi et al Inv Cph 1995; 36).
Furthermore cancer cells are undifferentiated – they act like foetal cells, being young and dividing rapidly and, as yet, not differentiated into lung cells, or liver cells or breast cells. Vitamin D can switch these undifferentiated cells over to being normal. And right now drugs companies are trying to patent drugs to do this! Why not just give people vitamin D supplements?!
Professor Michael Holick, an endocrinologist from The Boston University School of Medicine has argued that 25 per cent of the women who die of breast cancer would not have even had a problem if they had maintained adequate levels of vitamin D throughout their lives.
Black people, who cannot photosynthesise vitamin D under their pigmented skins, especially in our sunless European cities in winter, are known to develop more prostate cancers than caucasians and Gross (J Urol 1998) highlighted the use of vitamin D in the treatment of recurrent prostate cancer.
Vitamin D is claimed to greatly enhance radiotherapy effectiveness on breast cancer treatment (Mercola June 2003) – it is being used by the Royal Marsden for this very reason – and vitamin D is known to inhibit the growth of pre-malignant cells in the lining of the colon and reduces cancer tumours (Somer). In May 2003 at the Howard Hughes Medical School they showed that vitamin D detoxifies a carcinogenic bile acid Lithocholic acid, and confirmed that vitamin D can reduce polyps in the colon which often ultimately turn into cancer tumours.
Holick is clear that vitamin D reduces the risk of breast, colon and ovarian cancers, and named 13 others (from bladder to kidney to stomach) that he thought vitamin D could affect.
It seems, apart from these 16 cancers, scientists are discovering new health benefits almost daily for vitamin D with such illnesses as heart disease, diabetes, hypertension, auto-immune disease and even some mental illness and so-called SAD syndrome.
But What Is The Situation With Skin Cancer?
icons view is that although excess and burning sunshine can give rise to skin cancer, the charities that scare people against sunshine are doing the public a huge and dangerous dis-service.
Moreover there is actually research that endorses this view: The University of New Mexico (Journal of Nat Cancer Institute 2005, 97) has shown that its research findings conclude people with high exposure to the sun are less likely to die from melanomas. They too conclude vitamin D might be the protecting factor.
In our opinion the increasing levels of skin cancer and melanoma are largely due to increasing levels of endocrine-disrupting chemicals in the body and particularly on the skin, together with low levels of protective, antioxidant nutrients such as vitamins C, E, and omega-3 oils and minerals. One research study showed that with identical women, the one on the oestrogenic contraceptive pill had twice the risk of developing melanoma. Some sun screens have had chemical ingredients banned in Scandanavia as they mimic the action of oestrogen on the skin. And melanoma is driven by oestrogen, not simply excess sun light. New research in America is causing the FDA to rethink its stance on the ingredient retinyl palmitate, which seems capable of sensitising the skin and producing a greater skin cancer risk!
Conversely very recent evidence indicates that high blood levels of vitamin D actually help to prevent burning by speeding up tanning of the skin!
So what´s a girl (or a boy) to Do?
It is quite clear that every reader who is unable to achieve regular, gentle sun exposure would be well advised to supplement with a vitamin D3 supplement, at a dose of at least 400 IUs for prevention and 2,500 IUs to 5,000 IUs if they already have cancer. There are no reported contraindications with cancer drugs or cancer treatments in fact, exactly the opposite seems true.
Anybody with cancer, or at high risk of developing it, will do themselves no harm with a daily dose of up to 10,000 IUs, and may very well help themselves greatly. Some hospitals have been using vitamin D supplementation with breast cancer patients, and/or during radiotherapy, and/or as a part of a general programme of cancer therapy.
Worryingly, of course, we have had various EU directives which seem based on out of date research and/or subjectivity not science, and these seem bent on cutting RDAs for vitamins and supplements. In the case of vitamin D, RDA levels are much lower than all recent research would indicate to be essential. Recent research on vitamin D merely highlights the conflict that at the same time the bureaucrats are clamping down, the scientists are just discovering how these essential ingredients really work.
An Interview with John J. Cannell, M.D.
By Richard A. Passwater, Ph.D.
The Institute of Medicine (IOM) has published its new recommendation for the dietary intake of vitamin D. The new recommendations contain significant changes from IOM’s previous recommendations in 1997, and current research indicates that even the new changes are already out of date. During the next few months, we will chat with the executive director of The Vitamin D Council, John J. Cannell, M.D., about vitamin D and new research.
Many readers may already be familiar with Dr. Cannell’s impressive record of actively working to improve the health of all people—not just his own patients. We will discuss some of his efforts in a later installment, but let’s start with his educating physicians, scientists and the general population about vitamin D.
Dr. Cannell graduated with a degree in zoology from the University of Maryland, where he was a member of Phi Beta Kappa. He received his M.D. from the medical school at the University of North Carolina. After a year-long surgery internship at the University of Utah and four years of practicing itinerant emergency medicine, he began as a general practitioner in the coalfields of Appalachia.
Later, Dr. Cannell left general practice and went back to school to study psychiatry. He moved to Atascadero, CA, in the late 1990s and began working as a psychiatrist at Atascadero State Hospital, the largest hospital in America for the criminally insane. There, his long-held interest in clinical nutrition was re-awakened. The further he studied nutrition, the more and more vitamin D3(cholecalciferol) caught his attention.
As Dr. Cannell began to study the effects of vitamin D, he immediately realized that the recommendations of the Food and Nutrition Board (FNB) of the IOM were placing many Americans at risk. He found that vitamin D insufficiency was common in older adults, even using conservative cutoff points for vitamin D blood levels. Dr. Cannell was left wondering whom he should believe, Nature or the FNB? In 2003, he recruited professional colleagues, scientists and friends for a board of directors and took the steps necessary to incorporate The Vitamin D Council as a tax exempt, nonprofit, 501(c)(e) corporation.
In September 2006, Dr. Cannell’s seminal article, “Epidemic Influenza and Vitamin D” was published in the Journal of Epidemiology and Infection. The article presented a revolutionary new theory on vitamin D’s link to influenza and was co-written with some of the world’s top vitamin D experts.
Passwater: Dr. Cannell, why did you become interested in vitamin D?
Cannell: Ten years ago, I saw the possibility that vitamin D might radically change modern medical care. The reason I thought that was possible was, first, the mechanism of action of vitamin D, and second, the fact that people had suddenly stopped doing the things they needed to do to get vitamin D. Because of those two things, I realized that it might be possible to bring about a dramatic change in modern medical care.
Passwater: Well, vitamin D is indeed unique. What did you learn about this uniqueness?
Cannell: Historically, we didn’t depend on vitamin D in foods at all, but now we are increasingly becoming dependent on diet for vitamin D. Over the millennia, humans have gotten their vitamin D mostly from sunlight striking their bare skin. In order to make vitamin D, you must be outside when the sun is high enough overhead. If the sun is low on the horizon, you may tan but you won’t make much vitamin D.
Passwater: How is it made in the skin?
Cannell: The vitamin D precursor in our skin is 7-dehydrocholesterol, which is made in the body from cholesterol. ultraviolet-B (UVB) energy converts 7-dehydrocholesterol into cholecalciferol, which is the name of natural vitamin D. Cholecalciferol (pronounced koh· luh· kal· sif· uh· rawl) is then carried in the bloodstream to the liver, where it is converted into the prohormone 25-hydroxy vitamin D (calcidiol). Some of that 25-hydroxy vitamin D is then transported to the kidneys where it is hydroxylated further to form 1,25-hydroxy vitamin D (calcitriol). This form is the physiologically active form of vitamin D. The calcitriol made in the kidneys is to fulfill only one of vitamin D’s functions: its endocrine function, which is to maintain the calcium economy.
Technically not a “vitamin,” vitamin D is in a class by itself. Its second metabolic product, 1,25-hydroxy vitamin D (calcitriol), is actually a hormone, a key that fits binding sites on the human genome. The human genome contains more than 2,700 binding sites for 1,25-hydroxy vitamin D; those binding sites are near genes involved in virtually every known major disease of humans.
Passwater: No wonder vitamin D is the focus of so many disease-related studies. It seems to be involved in almost everything.
Getting back to the effect of position of the sun and the production of vitamin D, is this because it takes more UV energy (in terms of photons per unit of time or surface area) to convert 7-dehydrocholesterol to vitamin D, or does the conversion require a different energy in terms of wavelength?
Cannell: Vitamin D3 is made in the skin when 7-dehydrocholesterol reacts with UVB at wavelengths between 270 and 300 nm, with peak synthesis occurring between 295 and 297 nm. A large number of these wavelengths are present in sunlight when the sun is high enough that your shadow is shorter than you; otherwise, the ozone in the atmosphere prevents UVB radiation from penetrating the atmosphere.
Passwater: You mentioned that time of day is critical in producing vitamin D in skin, but latitude and time of year also play roles. At 42 degrees latitude, the sun’s energy at noon is only 75% of the energy at the equator (SIN 48) at that time. The noonday sun in Florida is more intense (i.e., more UV photons per square inch) than the noonday sun in New York, so New Yorkers need more time in the sun to make their vitamin D. A beam of noon sunlight is spread out further (thus has fewer photons of UV energy per square inch) in Chicago than in Peru. In Chicago, the noon sunlight is at 42 degrees north latitude and has an angle of 42 degrees; in Peru, the noon sunlight is at three degrees south latitude, which makes the sun angle 87 degrees.
Cannell: Yes, that’s right. Also, think of UVB photons as ping pong balls. They bounce around. They bounce off buildings, sand, water, even the bottom of clouds, until they hit something that absorbs them, like your skin. That’s why you can make vitamin D under a sun umbrella at the beach.
Passwater: Well, the sun and Earth haven’t changed much, and skin hasn’t changed much. What has changed?
Cannell: More people used to work outside, which enabled them to get plenty of vitamin D and store it up for the winter time. In the last 50 years, we started living inside virtually all the time. In the last 25 years, we basically stopped going out in the sun at all. People have changed their minds about the sun; it is now considered “evil.” When you and I were growing up, our mothers told us that sunshine and fresh air were good for us. You never hear that anymore. Now, sunshine is a bad thing!
That was just one of several things that occurred. Others were the introduction of indoor video games and the fear that children should not be outdoors because predators might abduct them. Then, there was the fear that the sun would damage the skin. All these things affected our society in dramatic ways.
Starting in the 1980s, for the first time in human history, doctors began telling patients to avoid the sun. Up until that time, the sun was recognized as a curative agent by every form of medicine known to man. Then, the American Medical Association and their Council for Scientific Affairs started saying something very different: the sun is harmful, stay away from it. It is interesting what they didn’t say: “By the way, since you are not going out in the sun, you need to take 5,000 units of vitamin D/day to make up for your lack of sun exposure.”
In fact, they actually said it won’t matter because vitamin D will remain the same whether or not you go in the sun, which is a patently absurd statement. So, I said to myself, with the dramatic change in sun exposure over the last 25 years, vitamin D levels must have fallen dramatically in at least some, but probably many, people.
Passwater: Your points are well taken. What was the second factor that aroused your concern about and interest in vitamin D?
Cannell: Vitamin D is not a vitamin; it is a seco-steroid hormone. It works by directly regulatingabout 1,000 human genes, which is about 5% of the human genome.
Passwater: Amazing! Thirty-five would be a very decent number of genes to regulate. Two hundred would be an enormous amount. But, 1,000 is mind-boggling!
Cannell: People sometimes think that their genes are inherited, carried around and then passed on to their children, which is all the genetics they know. They don’t think about what their genes do between the time they are inherited and the time they are passed on to their children. Genes are the brains of your body more than your brain is. You can only read this now because your genes are working, making the enzymes that the eyes and brain need to conduct the immensely complicated biochemical task we call reading.
In other words, your genes are regulating your body’s proteins including the enzymes and proteins involved in vision. Genes are the conductors that allow your brain to work as you read this.
A large percentage of the human genome, maybe up to 2,000 human genes when including indirect control, are controlled by vitamin D. Without vitamin D, those genes literally do not know what to do. They don’t know whether to increase or decrease the production of their particular enzyme. Vitamin D can turn a gene on or off. The genes don’t know what to do without vitamin D.
So, you can see that once you understand the mechanism of action of vitamin D (i.e., that it turns hundreds of genes on and off and regulates them), then you can say, “Oh, that’s the reason that vitamin D can be involved in the eyes in macular degeneration, and teeth as in dental caries, in the heart in heart attacks or involved in bone, breast, colon and prostate health, in the pancreas and diabetes and so on,” which brings us to the “triple-A epidemics” raging among our children: autism, asthma and autoimmune disorders.
In my opinion, vitamin D deficiency during pregnancy and early childhood is the principal cause, actually the principal trigger, of autism. There are doctors at Harvard who think childhood vitamin D deficiency is also the cause of the childhood asthma epidemic, and other doctors have written that vitamin D deficiency during pregnancy and early childhood is involved in the epidemic of autoimmune disorders such as insulin-dependent diabetes mellitus, which has increased dramatically among our children.
Passwater: Interesting observations indeed. We’ll certainly chat more about them in Part 3. So, we have a vitamin that is not a vitamin, but a very potent and multi functional hormone.
Cannell: Yes, vitamin D is like a key to a lock.
What vitamin D does is directly unlock about 1,000 human genes. This is even more curious in that it is dependent on human behavior. In all other cases that I can think of, something as important as vitamin D would never be left up to the choice of the organism. The human organism would evolve a way to make it if it was needed, without relying on human behavior. But if you need vitamin D, you can’t make it unless you do one thing: go outside and allow UVB radiation to strike your skin.
For millennia, we were never out of the sun. Humans were always in the sun. Nature could not conceive of the possibility that humans would banish sunshine. However, starting with the Industrial Revolution, we began working inside, but we still had vegetable gardens. We still walked around outside and rode horses. Then, cars came along and we started driving in vehicles with glass windows. Ordinary glass completely blocks UVB. Even if it is a very sunny day at solar noon, as you drive your car with your windows up, you’re not making a bit of vitamin D because of the glass.
Soon, more and more people came off the farm to work in factories. Even people who worked on farms started using tractors that had glass windows like cars. Changes kept occurring that reduced our UVB exposure and lowered vitamin D levels.
Then, came the three events that I already mentioned: the fear of child predators, video games and skin cancer, with the ultimate order by the American Medical Association (AMA) that pregnant women should not go out in the sun, mothers should not go out in the sun, children should not go out in the sun and adults should avoid the sun. If you had to go outside, always put on sunblock. I predict that particular piece of AMA advice will go down in history as the single most lethal piece of medical advice ever given.
Sunblock can be very effective in preventing vitamin D formation. The only good news is that very few people apply sunblock properly. You have to use a lot of it to block out all the UVB radiation. However, now people are using SPF 60 and 80, which means they’re very effective sunscreens.
So, what I realized was that intracellular levels of this substance—this steroid hormone called vitamin D—had been dramatically decreased in people over the last 25 years. At the same time, the “triple-A epidemics” began to occur among our children.
Passwater: You have been doing an excellent job of educating other scientists about these three new epidemics. You have put together many very interesting facts about vitamin D deficiency and autism. Our readers will certainly want to read Part Three of this article, where you tell us more about this.
Cannell: When I say epidemics, in 1970 it was rare to see a child with insulin-dependent diabetes mellitus, asthma or autism. Now, everybody knows kids with those disorders. It has increased dramatically and shows no sign of stopping. For example, the National Institutes of Health reported about nine months ago that if you have a male child born this year, that boy will have about a 1 in 60 chance of developing autism before he is eight years old. One in 60! It used to that a typical psychiatrist would never see a case of autism in his/her whole 40 years of practice.
Passwater: Well, we can see why you became interested in vitamin D. Why did you then go on and organize The Vitamin D Council?
Cannell: As you know, I have always been an activist on issues such as smoking, black lung disease, public education school reform and a number of other things. I realized that wholesale supplementation of a population of American citizens with vitamin D might do more good than all the doctors and hospitals combined. When I discovered that this was a possibility, I knew that I had to do something.
If you need to do something, you need resources. I started The Vitamin D Council with the help of a group of concerned citizens and scientists who believe many humans are needlessly suffering and dying from vitamin D deficiency. We have been incorporated as a nonprofit, tax-exempt 501(c)(e) educational corporation in the state of California since 2003.
Our goal is to educate the public and professionals about vitamin D deficiency and its numerous associated diseases. Our free Vitamin D Newsletter has a circulation of over 40,000 and is growing. The Vitamin D Council would like to sponsor a series of educational conferences aimed at the general public, physicians and the press to alert them about the extent and consequences of vitamin D deficiency and the simple steps that can be taken to avoid it.
Sometime in 2002, my son and I created The Vitamin D Council Web site,http://www.vitamindcouncil.org. This Web site now receives over 5,000 unique visitors each day. When someone does a vitamin D search on Google, our Web site usually is in the top three or so responses. We will have a brand new, radically different.
Passwater: You mentioned that vitamin D was unique in that it interacts directly with genes. Just how does vitamin D interact with the genome?
Cannell: The basic genomic interaction mechanism is fairly well known. Sitting on top of the genes to which vitamin D is responsive is something called the vitamin D response element. Close to the vitamin D response element is a vitamin D receptor. For vitamin D to work, it must combine with a molecule of vitamin A; this combination transforms the vitamin D receptor and locks onto the vitamin D response element. The gene then becomes activated (i.e., down-regulated/up-regulated or turned on/off).
Unfortunately, when some people hear or read that a molecule of vitamin A is also involved with vitamin D action, many people incorrectly assume that they should also take more vitamin A or cod liver oil. Don’t! I have written several papers about vitamin A toxicity in the United States. I think that retinol, the preformed vitamin A, is consumed in toxic amounts in this country. Humans have a profound ability to make all the preformed vitamin A that they need from the carotenoids found in colorful fruits and vegetables.
In fact, two molecules of vitamin A can combine to weakly stimulate the vitamin D receptor. This action of the combined vitamin A molecules blocks the desired strong interaction of the vitamin D–vitamin A combo. This, in essence, prevents the vitamin D mechanism from working. I find that the amounts of vitamin A consumed by humans in the United States are far greater than the vitamin D consumed. We consume much more vitamin A than experts think is healthy, yet the government doesn’t change its advice or take steps to reduce vitamin A fortification of food.
When you eat retinol—the preformed vitamin A that is found in foods such as eggs, liver, butter or milk—it is like injecting vitamin A directly into your vein. But, when you eat beta-carotene, it must go through your intestines and the intestinal cells will sense the amount of vitamin A in the blood. If you have enough vitamin A in your blood, your intestinal cells will not convert the beta-carotene into vitamin A. The beta-carotene or other carotenoids will not be converted into retinol, so the rate-limiting mechanism is in the intestine. If you take retinol, the preformed vitamin A, like in cod liver oil (not whole-body fish oil), you can easily reach harmful or toxic levels of vitamin A. Excessive vitamin A interferes with the action of vitamin D. Don’t take cod liver oil or supplements high in retinol, the preformed vitamin A. You can get all of vitamin A you need from colorful fruits and vegetables. Many supplements use beta-carotene as their source of vitamin A and this prevents the over-production of retinol in your body.
So, there’s plenty of vitamin A in your body for binding with vitamin D. It is the vitamin D molecules that are in short supply. When the two vitamin A and vitamin D molecules combine, they can activate the vitamin D response element and the gene becomes functional.
Passwater: Vitamin D functions by interacting with many hundreds of genes. Please explain to our readers the impact of this.
Cannell: It is really important for people to realize their genes control virtually everything. From your ears to your toes, everything depends on a complicated series of biochemical reactions that are occurring with the help of enzymes. Well, those enzymes are all activated by genes. For me to have the ability to talk to you now, it requires a functioning genome and your genome cannot function optimally unless you have enough vitamin D. It is the key that unlocks the hundreds of vitamin D-dependent genes that are locked away behind a vitamin D response element. It is crucial to understand that your genome is allowing you to live day to day.
Passwater: How about individual differences in vitamin D receptors, the widespread variations called single nuclear polymorphisms (SNP)? Are they an important factor?
Cannell: There are indeed SNPs. When mutations become so common that 10–20% of us have them, they’re no longer called mutations, but are called polymorphisms. There are many shapes of the vitamin D receptor. It appears that some of the vitamin D receptors are more functional than others, although this has never has been properly researched and it’s not clear what this means at this time. There is very little consistent SNP research on vitamin D receptor polymorphisms and the results are not clear at this time.
In all likelihood, variations in any polymorphisms in the vitamin D receptor simply mean more vitamin D is needed by some SNP to activate sufficient numbers of these receptors on the genes. All of the vitamin D receptor polymorphisms are functional; it is not as though some work and some don’t. However, variation in the functionality of these polymorphisms is one of the reasons why we recommend a 25-hydroxy-vitamin D level of 50 ng/ml in the blood rather than the IOM’s recommendation of 20 ng/ml. We want to be sure everyone gets a benefit.
Passwater: Dr. Cannell, how do we know how much vitamin D is required for our optimal health?
Cannell: We have learned a lot about this question by studying the amount of a compound called 25-hydroxy vitamin D (or 25-(OH)D). After vitamin D is formed in the skin or put in your mouth, it goes to the liver where it is hydroxylated by two enzymes to form 25-hydroxy vitamin D, which can be measured in the blood. This is used to determine vitamin D adequacy.
For years and years, the range in all major reference labs was about 20–100 ng/ml. It was found people having levels of 10 ng/ml or less often had rickets or osteomalacia, the adult form of rickets. So, 20 ng/ml is high enough not to get rickets, but 20 ng/ml is still on the low end.
On the other hand, we have lifeguards in Miami Beach in August who have levels near 100 ng/ml. This is high on the normal range of 20–100 ng/ml. As more and more research came out, the lower range moved from 20 to 25 to 30 ng/ml. Now, most labs list 30 ng/ml as the lower limit of normal.
So, the question is not what is the best vitamin D intake, but what is the ideal 25-hydroxy vitamin D level in the blood.
There are several ways to think about this. One is regarding public health for the entire population, understanding that the more melanin you have in your skin, the lower your vitamin D levels will be. Some people have so little melanin and are very efficient at making vitamin D that a short walk site to the mailbox will generate quite a bit.
But the more melanin you have in your skin, the lower the level of 25-hydroxy vitamin D you will have. So, when you think about a public health situation, you have to think about all these people who have very low levels such as African Americans. That’s one of the reasons that we recommend 5,000 international units (IU)/day because 95% of the people who take 5,000 IU of vitamin D/day will get the full health benefits of vitamin D and no one will get toxic effects.
Intake of 5,000 IU of vitamin D/day will generally lead to a 25-hydroxy vitamin D level of about 50–70 ng/ml, although that amount varies considerably from person to person. There’s a large genetic factor in the determination of your vitamin D level, and this surprises a lot of people. You inherit your vitamin D machinery and this affects how high or low your actual vitamin D level is in the blood. If you think about it in terms of public health involvement, it’s a Gaussian distribution where you want to shift the curve to the right so that nobody’s levels are down around 15 or 20 ng/ml; at the same time, nobody has levels of 150 ng/ml.
Levels of 90 ng/ml are ideal for one other reason. Think of vitamin D as being like a lake on top of a mountain. There are many streams that flow down the mountain from the lake. As you go down the mountain, there are hundreds of pools that are being fed by this lake at the top. When the lake gets low, the pools dry up. This is much like the way vitamin D synthesis works. Vitamin D in the form of 25-hydroxy vitamin D is the lake on top of the mountain. This lake is involved with calcium function, so the lake determines your blood calcium levels. This is a life or death situation as blood calcium must not fall too low or you die.
The primary function—and by primary, I mean the minute-to-minute life-sustaining function—of vitamin D is to maintain your serum calcium levels. Serum calcium is a cation that must be regulated precisely. If it goes up too high, you start calcifying your internal organs and you get cardiac arrhythmias; if it gets too low, you also get cardiac arrhythmias and all kinds of other problems. You can die from either too high or too low calcium levels in your blood.
If your body only has a little vitamin D, the lake won’t be dry, but it will be low with nothing left over for the streams and pools below. The pools lower down are those that we have been discovering over the last 10 years: the pools of autism, breast cancer, hypertension, congestive heart disease, diabetes, dental caries, macular degeneration, influenza and more. All these pools are underneath the primary lake of vitamin D. To get the full benefit of vitamin D, the lower pools as well as the lake above must be full. We don’t yet know exactly how high each pool must be, and we don’t know which pool is filled first, second or last.
Passwater: There is a similar hierarchy for selenium. The first priority for selenoproteins is for various general antioxidant defenses, the second hierarchy is for brain functions and the third priority—if there is any selenium still available—is for anti-cancer functions via apoptosis.
Cannell: We do know that there are 38 organs in the body that use vitamin D. Its need is certainly widespread. But, if you think about it that way, if you realize that we don’t have to know the details, and that all we need to know is that when all those pools are full, what happens? If all those pools are full, the body would start saving some of the vitamin D itself, not the 25-hydroxy vitamin D, for future use. This vitamin D is stored in muscles and fat.
Most people’s vitamin D level (not the 25-hydroxy vitamin D) in their blood it is almost zero! The levels are so low that they are undetectable. This implies that none of the 25-hydroxy vitamin D is getting all the way down the mountain. It is all being used up on the way down the mountain, so none of the vitamin D is being saved for the future.
Now, if you found someone who had a vitamin D level of 50 ng/ml, as well as a 25-hydroxy vitamin D level of 50 ng/ml, you could then say that this person definitely has enough vitamin D. He no longer suffers from what is called chronic substrate starvation. If your vitamin D level is zero—not the 25-hydroxy vitamin D level, but the vitamin D itself, which is something no one ever measures because it is very difficult to do—you are suffering from chronic substrate starvation by definition. None of the 25-hydroxy vitamin D got all the way down the mountain, so no vitamin D is being stored for the future.
Passwater: Chronic substrate starvation! Exactly what does the term mean? Vitamin D insufficiency?
Cannell: It means the substrate—in this case, vitamin D the building block, for the prohormone (25-hydroxy vitamin D) and active steroid (1,25-hydroxy vitamin D)—is in short supply and the body is starved for vitamin D.
There was an elegant study done by a researcher that I admire, Professor Robert Heaney, M.D., of Creighton University. He wanted to find out what level of 25-hydroxy vitamin D was needed to get vitamin D to be measurable in that person. He found that if your 25-hydroxy vitamin D level was 30 ng/ml, your vitamin D level was zero. That means if your 25-hydroxy vitamin D level is 30 ng/ml, not all the pools are full and you have chronic substrate starvation.
Passwater: But, don’t the new guidelines from the Institute of Medicine (IOM) recommend 20 ng/ml of 25-hydroxy vitamin D as being adequate? This recommendation would still result in chronic substrate starvation!
Cannell: Yes, it would. It is simply nonsense, and dangerous nonsense.
At around 30 ng/ml of 25-hydroxy vitamin D, about 25% of people started having detectable vitamin D levels in their blood. At 35 ng/ml 25-hydroxy vitamin D, half of the population will also have detectable amounts of vitamin D in their blood. If you get up to 50 ng/ml of 25-hydroxy vitamin D in your blood, then everyone has some detectable vitamin D in their blood as well, with more stored in their muscles and fat.
That means that if your blood level of 25-hydroxy vitamin D is 50 ng/ml or more, you will not have chronic substrate starvation. If your level is 35 ng/ml, you have a 50% chance of having chronic substrate deficiency. If it is 30 ng/ml, you have a 75% chance of having chronic substrate deficiency.
Passwater: Please remind our readers once again what is the practical health consequence of having chronic substrate starvation.
Cannell: It means the body does not have enough of one of the building blocks it needs—in this case, enough vitamin D—to meet the body’s needs.
Passwater: And, the IOM recommendation for blood level of 25-hydroxy vitamin D is what again?
Cannell: 20 ng/ml.
Passwater: There seems to be a disconnect between the facts and the IOM recommendations. Is the IOM committee unaware of Dr. Heaney’s findings?
Cannell: They are aware, but they were a political committee. For example, if they said 30 ng/ml, they would also have had to address food fortification, which they did not want to do. And, if they said 30 ng/ml, they would have had to make recommendations based on skin color, another politically impossible thing for them to do. (Very few Blacks have levels of 30 ng/ml, but about 50% of Whites do. So, by saying 20 ng/ml, they hoped to avoid the skin color issue.)
Passwater: You recommend between 50 and 90 ng/ml.
Cannell: Yes, about what people who work outdoors have in the summer.
You also have to ask the question, what group are we talking about. Is the person someone who is in apparent perfect health other than chronic substrate deficiency? If so, 50 ng/ml may be fine. Or, are we talking about a child with autism? In the case of autism, we want the level that helps the child.
Passwater: What I find interesting is that virtually all of the vitamin D researchers that I speak with all recommend 5,000 IU of supplemental vitamin D per day, the same as The Vitamin D Council.
Cannell: Yes. There’s an interesting article by Martin Mittelstaedt, who writes for the Toronto Globe and Mail, in which he polled vitamin D researchers. He asked them, “You have been doing vitamin D research. How much vitamin D do you take?” Do you know what the average was for the vitamin D researchers? 5,000 units a day.
Passwater: Well, that’s what I found, and recently several physician columnists who commented about the new IOM recommendations said they were taking 5,000 IU and were recommending between 2,000 and 5,000 IU for their patients.
Cannell: Yes. I find the same thing; even those who are recommending only 2,000 IU to their patients are taking 5,000 or 10,000 IU themselves.
Passwater: I’ve seen the same phenomenon over the years for other nutrients, especially the antioxidant nutrients. The thinking is something like, “Well, there isn’t enough absolutely conclusive evidence that this much is needed. But, I am very familiar with the vitamin D research and from what I am seeing, I want to take 5,000 IU for myself.” They are afraid that they will be criticized by anti-supplement forces that speak out against doctors who recommend supplements. So, they take the safe course and recommend what they can justify by conclusive evidence and then take what the leading edge of research suggests is right for themselves.
Most of our readers may be unaware that the FDA tried to limit the amount of vitamin D in dietary supplements to 400 IU and were pushing to even lower it further. On December 19, 1972, the FDA Commissioner, Alexander M. Schmidt, proposed, by publishing in the Federal Register, a regulation of the Food and Drug Administration that preparations of vitamin D in excess of 400 IU per dosage unit be restricted to prescription sale and that such dietary supplements be labeled accordingly.
Now how many people would that have harmed? If the body of scientific evidence shows that supplements of 5,000 IU are required to optimize blood levels of vitamin D, how many people would have been sentenced to cancer and various other diseases by this stupid and arbitrary action of the FDA?
Solgar submitted voluminous factual material and expert opinions opposing the proposed regulations to the FDA, but the FDA Commissioner ignored them and the regulation was promulgated on July 25, 1973 to become effective October 1, 1973. (38 Fed. Reg. 20723, 20725 (1973)) We took the Secretary of health, Casper Weinberger, and the FDA Commissioner, Alexander M. Schmidt, to court to have this action stopped.
At first, we (Solgar was now joined by NNFA) were not successful in the court and we had to appeal to United States Court of Appeals, second Circuit. Attorneys Milton Bass and Robert Ullman argued the appeal on October 19, 1973 and the court decided in our favor on December 11, 1973. Our industry was able to continue to provide products based on science to improve the health of people.
Another part of the story in learning about widespread vitamin D deficiency is that one of the most frequently used reference analytical laboratories that determine how much vitamin D is in patients’ blood was giving the wrong results. You uncovered this problem and led to having it corrected. Please tell our readers a little bit about this problem.
Cannell: I was the first to report that Quest Laboratories, the largest reference laboratory doing vitamin D analysis in the United States, was reporting incorrect results that made it appear the patients had more vitamin D than they actually did. Levels of 25-hydroxy vitamin D may have actually have been 20 ng/ml, but Quest was sometimes reporting it as twice that.
I reported this on-going error in my newsletter in July 2009. It was first picked up by Dr. Joseph Mercola, D.O., and then a trade journal for reference laboratories reported on it. Then, The New York Times reported it in December 2009. Quest then announced that they fixed the problem.
One of the things that The Vitamin D Council does is to check on laboratory results. We are doing a study in which we have asked our readers to have their blood analyzed for 25-hydroxy vitamin D by two different laboratories on the same day. We asked our readers to have their blood drawn and sent to Quest and then have it drawn again the same day and sent to LabCorp. LabCorp uses a technique that is the standard in the field. So, we are seeing whether or not Quest has solved its analytical problem.
Passwater: What was the nature of the problem? Was it an extraction problem?
Cannell: Yes. As you know, you have to prepare your sample specimen extremely carefully. This technique requires a highly skilled operator, who often holds a Ph.D. When vitamin D tests became the single most-requested lab test in the country, which happened about a year-and-a-half ago, the number of requests that Quest was getting for vitamin D increased 100-fold. You can’t rush the test with the procedure that Quest was using. Basically, it is a research method used to identify substances in blood. In contrast, the technique used by other reference labs is a simplified, fool-proof method. The standard technique is mechanized, more like most laboratory tests, and it doesn’t require an especially skilled operator. It can be done by most technicians.
Once that huge upswing in demand for vitamin D testing occurred, you can imagine the effect it had on the operators of this highly specialized instrument Quest uses. There were thousands of blood samples waiting for the analyst to run. You can guess what happens then. They’re human beings and they may rush the procedure to get everyone’s tests done. They don’t want to face a big backlog every day. When the procedure is rushed, the extraction is incomplete and not representative of the amount in the sample.
Passwater: How did you uncover the testing problem?
Cannell: I used to work in a state forensic hospital, where patients would come out of solitary confinement from prisons and would be checked out by us because they often became psychotic. We knew that they were not getting any sun. Even the hour that they were sent outside to exercise was in a shaded area was not enough to give them adequate vitamin D, especially the darker skinned inmates. The Quest results said that their 25-hydroxy vitamin D levels were fine and I knew they were not. I knew the Quest results were impossible.
There is a need to have vitamin D tests done so that doctors can learn how small of a dose 5,000 IU is. The only way that doctors can learn that lesson is to have a vitamin D test, give 1,000 IU/day and then be surprised that nothing much happens. Next, give 2,000 IU/day; the blood level may go up a little bit in the spring, but in the fall or winter, the level may actually go down. That is because of the overpowering effect that the sun has on vitamin D levels. The decrease in UVB radiation during the autumn overpowered the effect of the 2,000 IU per day.
Passwater: Didn’t this huge demand for vitamin D testing result in a move by the insurance companies to discourage them?
Cannell: There have been attempts by two different Medicare Regional Districts to stop paying for vitamin D tests. The Vitamin D Council was involved in fighting back through letter-writing campaigns. So far, we have been successful in fighting back those attempts, as far as I know.
Passwater: Many doctors practice defensive medicine and hesitate to recommend supplements unless they have laboratory evidence of deficiency.
Cannell: That’s a big part of the problem. However, the fact is that vitamin D blood tests really aren’t needed. All you have to do is to take 5,000 IU daily. I say they are not needed because if the doctors and patients are really knowledgeable about vitamin D, about the physiology and pharmacology, they know 5,000 IU/day is not very much. The problem is that the patients seem to think that 5,000 IU is a lot.
Passwater: Is this because they think 5,000 is a large number?
Cannell: Yes, but it is not a large amount by weight. The trouble is that 5,000 IU is only an eighth of a milligram of cholecalciferol; that’s only 125 micrograms. Micrograms, not milligrams! There are 1,000 micrograms in a milligram. When I explain to them how 5,000 IU actually is 125 mcg, they say, “Well, I’ll take that.”
Passwater: Yes, the average person can find the conventional systems for expressing quantities of nutrients to be confusing—USP Units, International Units, enzyme units, grams, milligrams, micrograms, etc.
The system of using standardized units was developed to measure biochemical activity long before the structure of the nutrient was determined. Not all International Units correspond to the same weight of a given nutrient. As an example, 1IU of vitamin E can be 0.671 mg of natural (RRR-alpha-tocopherol or d-alpha-tocopherol) vitamin E, or Y mg of synthetic (all-racemic- alpha tocopherol or dl- alpha-tocopherol) vitamin E, or 0.735 mg of d-alpha-tocopheryl acetate, or Z mg of gamma-tocopherol. International Units for the various vitamins are not the same weight units and they are not directly interchangeable. They must be converted to weight measurements for meaningful comparisons.
The international unit for vitamin D activity dates back before 1931 and was based on theantirachitic activity for the rat.
One thousand IU of vitamin D is only25 mcg of cholecalciferol and the same 25 mcg for the other form of vitamin D, the irradiated analog whose patent has expired, ergocalciferol (also called vitamin D2).
After a doctor becomes familiar with the pharmacology of vitamin D, all that has to be done when a patient comes in is to look at his/her skin type, look at the amount of melanin in the skin, ask about his sun behavior, what kind of job he has, does he have a covered garage, does he get up in the morning and put on his sun block, drive his car to work, etc. If the patient works inside, wears sunblock, and doesn’t take any vitamin D, he has a 100% chance of being vitamin D deficient. He doesn’t need a blood test.
So, 5,000 IU isn’t a lot of vitamin D and a lot of physicians and vitamin D researchers agree with your recommendation. Next month, we can chat a little bit about the safety/toxicity facts and how the U.S. Food Administration was pushing to lower the allowed amount of vitamin D in supplements to 200 IU in the 1980s.
Last month, we discussed how and why many vitamin researchers conclude that the best way to determine vitamin D adequacy is to measure the amount of 25-hydroxy vitamin D in the blood.
An intake of 5,000 IU of vitamin D/day will generally lead to a 25-hydroxy vitamin D level of about 50–70 ng/ml, although that amount varies considerably from person to person. A study done by Professor Robert Heaney, M.D., of Creighton University showed that if one’s 25-hydroxy vitamin D level was 30 ng/ml, his/her vitamin D level was zero.
At around 30 ng/ml of 25-hydroxy vitamin D, about 25% of people started having detectable vitamin D levels in their blood. At 35 ng/ml 25-hydroxy vitamin D, half of the population will also have detectable amounts of vitamin D in their blood. At 50 ng/ml of 25-hydroxy vitamin D in the blood, everyone has some detectable vitamin D in their blood as well, with more stored in their muscles and fat.
That means that if your blood level of 25-hydroxy vitamin D is 50 ng/ml or more, you will not have chronic substrate starvation. If your level is 35 ng/ml, you have a 50% chance of having chronic substrate deficiency. If it is 30 ng/ml, you have a 75% chance of having chronic substrate deficiency. The results of Dr. Heaney’s study are graphed in Figure 1.
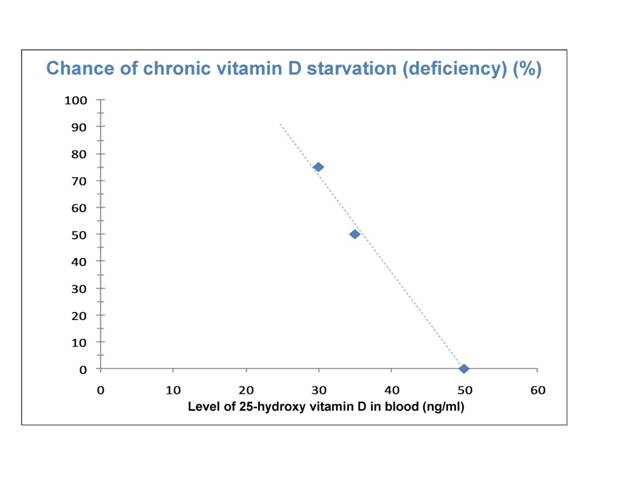
Figure 1: Three measurements of blood 25-hydroxy vitamin D are plotted against their corresponding chance of chronic vitamin D starvation (deficiency). Note that the 50 ng/ml recommendation of blood 25-hydroxy vitamin D recommended by Dr. Cannell and many researchers results in no chance of substrate starvation, whereas extrapolations to 20 ng/ml of blood 25-hydroxy vitamin D suggests that there is a large chance of substrate starvation. Even though extrapolations beyond measured points are uncertain, the last measured point at 30 ng/ml of 25-hydroxy vitamin D in the blood already is at the 75% chance.
Passwater: Dr. Cannell, you and many, if not most, vitamin D researchers are convinced by the body of scientific evidence that 5,000 IU of vitamin D should be the recommended intake for optimal health. Previously, people had been led to believe that only 400 IU was adequate. Now, when people read recommendations for 5,000 IU, they worry that this larger amount may be harmful. Perhaps, 5,000 IU seems to be a large number to them.
Cannell: It is larger than 400, but in the case of vitamin D, 5,000 IU is only an eighth of a milligram of cholecalciferol; that’s only 125 micrograms. Micrograms, not milligrams! There are 1,000 micrograms in a milligram. Perhaps if the dosage was stated in micrograms, they wouldn’t worry.
Passwater: Last month, we discussed that in 1972, the U.S. Food and Drug Administration (FDA) was trying to lower the amount of vitamin D available in supplements to 400 IU because of the FDA’s “concerns” that more would be toxic. How do you respond to those who remark that at 5,000 IU, vitamin D is toxic?
Cannell: They might think it’s toxic, but they can’t find a case in the medical literature in the history of the world that shows it is. They can’t even find a case of where somebody taking 10,000 IU of vitamin D a day—for no matter how many years—caused vitamin D toxicity.
Passwater: That was true in 1972 when the FDA tried to ban any supplement having more than 400 IU (making them available by prescription only) and in 1986 when I reviewed vitamin D safety in this column (1).
Where does vitamin D intoxication begin?
Cannell: Vitamin D toxicity would generally start to appear if someone was taking 50,000 IU a day for many months. Even in that case, 50,000 IU a day won’t be toxic for everybody. Vitamin D toxicity has never been documented to occur at blood levels less than 200 ng/ml.
When you say toxicity, people have these visions of being in intensive care units and vomiting and heart arrhythmias, and so forth. The first sign of vitamin D toxicity doesn’t mean that at all. It merely means that you feel perfectly fine, but when you have a blood test, your calcium level is slightly elevated. This is what I mean when I say the beginning of vitamin D toxicity. It is asymptomatic hypercalcemia.
At this level, it would take years and years to injure yourself.
One way to think about it is like water. If you go to your doctor and ask, “Doctor, have you ever heard of or seen a patient who has died from drinking too much water?” Virtually every doctor will say “yes.” Water intoxication is not uncommon. It is common in psychiatric patients and in long-distance runners who have this huge amount of water in their backpacks and they drink too much. It can cause swelling in the brain and seizures and death. There are hundreds of cases of people dying every year in the United States from water intoxication. However, you will never meet a doctor who has ever seen anybody die from vitamin D intoxication, unless you are at one of three universities that I am aware of that have reported it. It is that uncommon. Very uncommon!
Passwater: The Institute of Medicine (IOM) whose Food and Nutrition Board sets the diet recommendations (Dietary Recommended Intakes) defines its Tolerable Upper Intake Level (UL) as the highest level of daily nutrient intake that is likely to pose no risk of adverse health effects to almost all individuals in the general population. The UL represents total intake from food, water and supplements. Last year, the IOM raised its UL for vitamin D to 4,000 IU, whereas the Vitamin D Council puts its at 10,000 IU.
Cannell: Yes, we say the upper safe limit should be 20,000 IU. People have to understand what that means. The safe upper limit is the amount that anybody can safely take without seeing a doctor and without having any fear that they will be doing themselves any harm. It is the level that is safe for healthy individuals to take. However, if you have sarcoidosis (a systemic disease that is characterized by the formation of small grainy lumps in affected tissue) and you take 10,000 IU per day, then you may get profoundly hypercalcemic. But, that’s not vitamin D toxicity. The toxicity is from the sarcoidosis, not the vitamin D.
One good thing the Institute of Medicine did in its 2010 report was to change the UL from 2,000 to 4,000 IU. Vitamin D researchers all around the country had been plagued by the former UL of 2,000 IU as they often could not get approval to use more than 2,000 IU of vitamin D for treatment from the various safety and ethics committees that overlook research. Now, they will be able to see an effect from treatment with 4,000 IU thanks to the higher official UL.
It’s unfortunate that the IOM didn’t raise the DRI significantly. An interesting inconsistency is that it recommends 400 IU for a newborn infant and 600 IU for an adult woman, pregnant or not. Think about it. The IOM is recommending 400 IU for a five- or six-pound infant (80–67 IU per pound) and even for a 200-pound pregnant woman, it is recommending only about 3 IU per pound or about 125th the amount. The mother and baby inside the mother need 600 IU and the baby alone needs 400 IU. The IOM is suggesting that the 195 pounds of the mother alone needs only 200 IU of vitamin D, which is about 1 IU per pound. But as soon as the baby is born, the combination needs 1,000 IU of vitamin D. My contention is that if the mother and baby need 1,000 IU as soon as the baby is born, then they also needed it when the baby was still within the mother.
Passwater: The new report made a couple of small strides forward, but I felt the IOM was trying to save face with old recommendations and wanted to take only small steps. I know that a couple of researchers on the committee wanted to take larger steps forward.
Cannell: One of the problems with the structure of the IOM committee is that if you served on the previous committee, you can’t serve on the new committee. This means that some long-time experts in vitamin D research could not be members now. Another problem of the committees is that the dissenting viewpoints are not published. You don’t even know how much dissension there was or how close the votes were. In fact, they don’t pick “vitamin D experts”; they pick “scientists.” Of the dozen scientists on the vitamin D committee, only three had extensive experience in vitamin D research.
Passwater: The Committee needs to take steps that are more in line with the recent steps taken by several editors of medical journals towards full disclosure.
Cannell: Yes, there even was a conflict of interest that has not been widely talked about. One of the scientists on the Board (or Committee) had financial interest in what are called vitamin D analogs. Here’s how the system works. Natural compounds can’t be patented. If one takes the vitamin D molecule and changes it somehow such as adding on another element, one can get a patent on the new variation. All that one has to do is make sure it doesn’t completely lose its effectiveness and that it is not a naturally occurring substance. Then, one can do a study and compare it with a placebo—not natural vitamin D—and obtain a use patent and apply for a new drug. This is what happened with one of the members and his university. They patented ergocalciferol and continued funding the research with this compound they also called vitamin D. The same has been done with analogs of the active hormone, 1,25-hydroxy vitamin D. Instead of studies being funded comparing these expensive patentable compounds (drugs) with inexpensive natural vitamin D against various diseases, they compare these drugs with placebo.
Some members of the Board as well as their scientific advisors would have adverse financial effects if plain, old, inexpensive natural vitamin D was shown to be better than the patented drugs. I know that these are ethical scientists who believe in what they’re doing, but these sorts of conflicts should be disclosed. I didn’t see anything in the IOM report wherein any scientist disclosed any possible conflict of interest.
Passwater: It is a perverse situation. Now that we have covered how vitamin D works in the body and the recommended dosages for optimal health, I want to move on to your research. Let’s take another break and resume next month with your research and lead up to your new hypothesis about vitamin D insufficiency triggering autism.
Passwater: Dr. Cannell, I believe that your study about vitamin D protecting against the flu was responsible for many researchers becoming interested in also studying vitamin D. This is indeed a very important study. Please give our readers some of the background for your study.
Cannell: In the spring of 2006, an influenza outbreak occurred at the Atascadero State Hospital where I used to work, Now at that time, I had all of my patients on vitamin D, usually 5,000 IU a day, I watched as the influenza outbreak closed one ward after the other at the hospital. We had about 30 wards at the hospital. They closed the ward to my right, the ward across the hall and the ward to my left; all were quarantined because of influenza. I knew my patients had been exposed because they shared courtyards and other common areas together. Plus, I knew that my nurses had been exposed, and all of my nurses were on vitamin D at the time. They had worked with me and had seen the benefits of it. I watched and my patients didn’t get sick.
I started writing about this. I realized what I needed was to research the literature. In researching the literature, I came across a really interesting man, and I say that somewhat narcissistically because he reminds me a little of myself in some ways. Of course, I am not anywhere as near as brilliant as he was. His name is Dr. Robert Edgar Hope-Simpson.
Passwater: The British Medical Journal called him one of the most brilliant general practitioner researchers of the 20th century (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC261759/). He was most noted for elucidating the relationship between chicken pox and shingles. After his death in 2003, an article in the British Medical Journal remarked, “Only a great intellect could have conceived the possibility that, remarkably, a virus could commonly lie dormant in the human body, for years, indeed decades, and then reappear in another form. Only an unusually determined researcher could have pursued the idea through fieldwork in the natural history tradition.”
Cannell: Yes, he discovered the etiology of shingles just by thinking about it and then doing some tests on patients. It was just remarkable. He dedicated the last 25 years of his life to studying influenza because it is the one infectious disease that has the ability to bring the world to its knees. It has in the past with devastating epidemics like the one that occurred in 1919.
I kept reading the literature and then I contacted other researchers including Dr. Ed Giovannucci, M.D., Sc.D., professor of nutrition and epidemiology at Harvard. I wrote a draft and sent it to others in the field that would revise it and then I would send the updated draft to others who also became co-authors. Eventually, we published the first article that implied vitamin D might be helpful and that vitamin D was important in explaining the many mysteries surrounding influenza (1).
Passwater: What did Dr. Hope-Simpson write that stimulated your thinking about vitamin D and the flu?
Cannell: What Dr. Hope-Simpson pointed out was that sunlight might be involved in influenza. When he looked at the latitudes and the sun exposures, he concluded that there was a factor in this that had to do with the sun. He called it the solar factor. Dr. Hope-Simpson wrote in 1981, “Outbreaks are globally ubiquitous and epidemic loci move smoothly to and fro across the surface of the earth almost every year in a sinuous curve that runs parallel with the midsummer curve of vertical solar radiation, but lags about six months behind it … Latitude alone broadly determines the timing of the epidemics in the annual cycle, a relationship that suggests a rather direct effect of some component of solar radiation acting positively or negatively upon the virus, the human host, or their interaction (2).”
Passwater: That reminds me of Drs. Cedric and Frank Garland and their work with vitamin D and colon cancer.
Cannell: It seems fairly obvious, but I have been working at this for 10 years with influenza and the message is still not getting through to many physicians. The Drs. Garlands have been trying to educate people about vitamin D and colon cancer for 30 years and the wait goes on.
Passwater: Your vitamin D and influenza paper did, however, get the attention of many scientists.
Cannell: It has been cited several hundred times in other scientific publications. We have since updated and expanded on the seminal paper with a review published in Virology Journal (3).
Passwater: In your seminal paper in 2006, you proposed that vitamin D was the “seasonal stimulus” elucidated by Dr. Hope-Simpson. You presented graphical data correlating flu incidence with average 25-hydroxy vitamin D levels in the blood. You also described a paper that directly examined the relationship between vitamin D and respiratory infections. Dr. P. Rehman gave 60,000 IU of vitamin D a week and 650 mg of calcium daily for six weeks to 27 non-rachitic children (aged 3–12 years) who were also suffering from frequent childhood infections, mostly respiratory infections (4). Dr. Rehman found, “no recurrences were reported for a period of six months, in the treated children.”
Please tell our readers about the questions that Dr. Hope-Simpson asked about the nature of influenza.
Cannell: As we pointed out in the Virology Journal publication, perhaps the most universally accepted assumption about influenza is that it is a highly infectious virus spread by the sick. Dr. Hope-Simpson not only questioned that assumption, but he also went much further. Realizing that solar radiation has profound effects on influenza, he added an unidentified “seasonal stimulus” to the core of his epidemiological model. Unfortunately, the mechanism of action of the “seasonal stimulus” eluded him in life and his theory languished. Nevertheless, he parsimoniously used latent asymptomatic infectors and an unidentified “season stimulus” to fully or partially explain seven epidemiological conundrums:
- Why is influenza both seasonal and ubiquitous and where is the virus between epidemics?
- Why are the epidemics so explosive?
- Why do epidemics end so abruptly?
- What explains the frequent coincidental timing of epidemics in countries of similar latitudes?
- Why is the serial interval obscure?
- Why is the secondary attack rate so low?
- Why did epidemics in previous ages spread so rapidly, despite the lack of modern transport?
In our 2008 publication, we added an eighth conundrum—one not addressed by Dr. Hope-Simpson: Is the surprising percentage of seronegative volunteers who either escape infection or develop only minor illness after being experimentally inoculated with a novel influenza virus?
The percentage of subjects sickened by iatrogenic aerosol inoculation of influenza virus is less than 50%, although such experiments depend on the dose of virus used. Only three of eight subjects without pre-existing antibodies developed illness after aerosol inhalation of a flu virus. Intranasal administration of various wild viruses to seronegative volunteers only resulted in constitutional symptoms 60% of the time; inoculation with Fort Dix Swine virus (H1N1)—a virus thought to be similar to the 1918 virus—in six seronegative volunteers failed to produce any serious illness, with one volunteer suffering moderate illness, three mild, one very mild and one no illness at all. Similar studies on other H1N1 viruses found 46 of 55 directly inoculated volunteers failed to develop constitutional symptoms. If influenza is highly infectious, why doesn’t direct inoculation of a novel virus cause universal illness in seronegative volunteers?
We also added a ninth conundrum in the 2008 publication. Epidemiological studies question vaccine effectiveness, contrary to randomized controlled trials, which show vaccines to be effective. For example, influenza mortality and hospitalization rates for older Americans significantly increased in the 80s and 90s, during the same time that influenza vaccination rates for elderly Americans dramatically increased. Even when aging of the population is accounted for, death rates of the most immunized age group did not decline. Rizzo and colleagues studying Italian elderly, concluded, “We found no evidence of reduction in influenza-related mortality in the last 15 years, despite the concomitant increase of influenza vaccination coverage from ~10% to ~60%” (5). Given that influenza vaccinations increase adaptive immunity, why don’t epidemiological studies show increasing vaccination rates are translating into decreasing illness?
Passwater: What were the explanations presented in your articles?
Cannell: As we published in our 2006 paper, the compelling epidemiological evidence indicates vitamin D deficiency is the “seasonal stimulus” suggested by Dr. Hope-Simpson. Furthermore, recent evidence confirms that lower respiratory tract infections are more frequent, sometimes dramatically so, in those with low 25(OH)D levels (6–8).
In 1992, Dr. Hope-Simpson predicted, “Understanding the mechanism (of the seasonal stimulus) may be of critical value in designing prophylaxis against the disease.” Twenty-five years later, Drs. Aloia and Li-Ng found 2,000 IU of vitamin D per day abolished the seasonality of influenza and dramatically reduced its self-reported incidence (9).
Passwater: What biochemical mechanism is involved in vitamin D’s protection against the flu?
Cannell: It’s really neat. Several vitamin D response elements (see Part 2) are sitting on genes that regulate the production of antimicrobial peptides. Recently it has been shown that 1,25(OH)2D dramatically stimulates genetic expression of antimicrobial peptides (10–12). Antimicrobial peptides are the very simple, very potent naturally occurring antibiotics that our bodies make. They are made by our immune system cells as well as by our epithelial cells that line our throat, respiratory tract and intestines. They exist in immune system cells including neutrophils, monocytes and natural killer cells. In the epithelial cells lining the respiratory tract, they play a major role in protecting the lung from infection. They are part of what is called the innate immune system. They’re rapid action. They’re ready to go in milliseconds of a virus penetrating the mucus of the respiratory tract. They don’t need to be primed with an antibody like the acquired immune system does. The antimicrobial peptides are useful not only in killing the bacteria, but also in regulating the immune response.
One of the reasons that so many young people died in the 1919 epidemic was once the 1919 virus infected you, it made you sick, but your immune system would make you even sicker because it would mount this inappropriate all-out attack that killed not just the virus, but also many of the respiratory cells in your respiratory tract. The victims had their respiratory tracts denuded of epithelial cells. Doctors had never seen this before.
Vitamin D works in many ways in the immune system. Antimicrobial peptide production is just one of them. What vitamin D does is make your immune system smarter, not stronger. If your immune system becomes too strong, you can get autoimmune diseases. What is important about vitamin D is that it makes your immune system smarter.
What I used to do with the Vitamin D Council back in the days when there was just one article being published in the scientific literature every week or so—now there are hundreds every month—I would write a newsletter about each new study. Now, I can’t do that because there are too many new studies.
One of the highlights of my scientific career is that within days of my first influenza paper on vitamin D and influenza being published in England in the journal Epidemiology and Infection—which is the same journal that Dr. Hope-Simpson published in—the editor received a letter from Dr. John Aloia’s research group in New York. The group had been doing a vitamin D study in bone and by chance, one of the questions they happened to ask the patients in their study was, “Had you had any symptoms of a cold or flu within the last month?” When Dr. John Aloia read my paper, and then looked at his data. Lo and behold, the women he had on vitamin D were much less likely to get a cold or flu. He wrote that as a letter to editor announcing his findings (13). It is very unusual for a theory to get supportive evidence so quickly. Now, the theory basically has been accepted as true by many. Of course, nothing can be proven to be true.
Passwater: And, we can all put that knowledge to practical use immediately as there are other health benefits from 5,000 IU of vitamin D daily in addition to reducing the incidence of influenza.
Passwater: You mentioned you were an admirer of Dr. Robert Edgar Hope-Simpson because of the brilliant manner in which he could analyze facts about the incidence of diseases and elucidate their real causes. You have proposed very reasonable hypothesis about the etiology of several modern diseases and vitamin D deficiency. Last month we discussed the compelling and convincing evidence in support of your hypothesis that vitamin D is protective against influenza. This month, we will discuss your observations that link vitamin D deficiency as a trigger for autism and other childhood diseases of modern civilization. But first, I want to explore how your thinking – like that of Dr. Hope-Simpson’s — pieces the facts together and gleans what others have missed.
Please tell us more about how you pieced together the etiology of influenza and vitamin D deficiency for your seminal paper in 2006. There is a great similarity between your approach to influenza, autism, asthma and autoimmune disorders such as insulin-dependent diabetes mellitus. You have pointed out that these are the “triple-A epidemics” now raging among our children.
In Part One, you stated that in your opinion, vitamin D deficiency during pregnancy and early childhood is the principal trigger of these “Triple A” diseases that have increased so dramatically among our children.
Cannell: As I mentioned last month, I had been routinely giving all of my ward patients vitamin D supplements to help with their general health. It then became obvious to me no patient in my ward or care-givers developed influenza in spite of the epidemic in all the other wards. Influenza is not always just a miserable case of the flu; it can spread quickly and kill thousands. So I began thinking about vitamin D and influenza. I had extensive knowledge of vitamin D biochemistry, but little more knowledge about influenza than what is taught in medical school.
I then started reading the medical literature in depth, everything I could find about influenza. When I read the epidemiology of influenza papers especially, it just fit!
Everything just fit! Blacks were more likely than whites to get influenza. Blacks were more likely to get sicker when they get the flu. The closer to the equator you live, the less likely you were to die from influenza. The further away one lives from the equator, the more severe the attacks. The epidemics come in the wintertime and go away in the summertime. People who get more sun exposure don’t get as much influenza. Everything fit!
But all of these observed facts had been explained away in different or alternative ways. Children with rickets frequently get influenza. That was explained away as being because their rib cages were too soft. Or, that people got more influenza in winter because they were in closer contact. Every one of these observed facts that I read about had a different explanation. All twenty different facts had twenty different explanations, but, vitamin D deficiency explained each and every single fact. It is a key observation when one thing explains all observed facts. It is a parsimonious theory when one thing explains all the facts.
Passwater: It definitely increases the probability that the theory is correct.
Cannell: After I realized the relationship between vitamin D deficiency and influenza, in the back of my mind, I started thinking about autism as well.
Passwater: The two diseases are strikingly different. It would be surprising if they have the same trigger or co-factor. We all know what influenza is, and most of us think we know what autism is. But, for the record, just what is autism?
Cannell: Autism is just one disorder of a group of similar disorders called Autism Spectrum Disorders (ASD). ASDs are a group of developmental disabilities characterized by atypical development in socialization, communication, and behavior. ASDs typically are apparent before age 3 years, with associated impairments affecting multiple areas of a person’s life. Autism affects both the brain and body of young children. There are no biologic marker exists for ASDs, thus, identification is made by professionals who evaluate a child’s developmental progress to identify the presence of developmental disorders.
In 2009, approximately 1% of all children or one child in every 110 was classified as having an ASD. This percentage has been increasing steadily over the years as shown in Figure 2.
Figure 2: Autism prevalence. Percent children born with autism in USA. The actual numbers may be skewed somewhat do to reclassification adjustments and the awareness of autism changing a few diagnosis which in earlier years may have been “retardation” to “ASD” due to more accurate definitions and diagnosis.
I’m a psychiatrist so I knew quite a bit about autism. I could see that some of the observed facts about autism also were explained by vitamin D deficiency much like influenza was.
My current patients were adults, so I had to catch up on the more recent medical literature on autism. Again I found that observed fact after fact fit the vitamin D deficiency hypothesis. There is an increased prevalence of autism with increasing latitude. Autistic children tend to be less symptomatic in the summertime and more symptomatic in the wintertime. Black children are more likely to be autistic than white children. Somali immigrant children to Minnesota and Sweden were much, much more likely to get autism than those in their native country. People with more sun exposure were less likely to get autism. There was a seasonal variation children born from a winter’s gestation were much more likely to get autism than children born from a summer’s gestation. Mothers who are in higher socioeconomic incomes with higher education are more likely to have a child with autism. That’s always been a mystery but such parents are much more likely to use sunblock. In most diseases, that’s usually the opposite – the poorer you are and the less educated you are, the more likely you are to get a disease.
Passwater: Yes, that is surprising. What is the link?
Cannell: What’s the group of people most likely to put sunblock on their children and most likely to avoid the sun.
Passwater: The rich and educated. I now see the link, too. Would that also explain why there seems to be an association, like with Down’s syndrome, between the mother’s age and incidence of autism? Don’t older mothers tend to also be better off socioeconomically and educated more to use sunblock, etc.? Some may be career women who postponed child-rearing until a later time and they became vitamin D deficient while working indoors.
Cannell: Bingo! I suspect older women are richer and more likely to use sunblock but I am unaware that this has been proven true.
When I started first proposed my theory on vitamin D deficiency and autism, I proposed it on my website (1.Cannell, J. J. Autism and vitamin D. The Vitamin D Newsletter. 2007 May) before I published it in the peer-reviewed scientific literature (2.Cannell, J. J. Autism and vitamin D. Med Hypotheses. 2008; 70 (4): 750-9.). It just went nuts!
The mercury immunization theory backers sent me hate mail. I had never seen anything like it before. Especially since I was proposing that if you get these children on adequate amounts of vitamin D supplements quickly enough, you may be able to protect their brains. It was incredible.
One thing that people should realize is that if you have a child with autism, statistically speaking, your family is in more distress than if you have a child with a fatal illness. If you have a child with brain cancer, it is easier on the family than if you have a child with autism. It is an incredibly disruptive disease to family life. Because it’s not just the child banging his head on the TV set or screaming at three o’clock in the morning It’s the worry of what’s going to happen to my child when I’m gone.
Then the immunization/vaccine theory came out and it helped these parents because it resolved these parents of blame. The immunization theory meant that these parents could say that it was nothing that I did wrong. It was big pharma and the medical system and the vaccine industry that did this to my child. I didn’t have anything to do with it – they did it. I didn’t do anything wrong. It is a very important thing to believe if you have a child who has a disease as serious as autism.
My vitamin D deficiency theory is a little bit different. My theory says that if the mother had gone out and sun bathed, her child wouldn’t have autism. So mothers could easily see that as “blame the mother.” But, of course, if she had gone out and sun bathed while she was pregnant, she would be violating all of advice given by every major medical organization in the world. Mothers should not blame themselves! They’re only doing what the doctors told them to do. It’s not their fault at all.
In large part due to autism, I predict that the advice that was given by the American Medical Association in 1988 to always avoid the sun unless you are wearing sun block will turn out to be the worst medical advice ever given in the history of mankind!
I say that because there has never been blanket advice given that has caused so much death and suffering as that advice.
Passwater: Doesn’t a study of multivitamin use and autism give some support to your theory? The study showed that prenatal multivitamins, which typically contain 200 – 400 IU of vitamin D, reduced the incidence of autism. (Irva Hertz-Picciotto et al., July 2011 Epidemiology). Women who did not take a daily prenatal dietary supplement three months before and during the first month of pregnancy were almost twice as likely to have children with autism spectrum disorders, compared to those who started such a supplementation schedule early.
Cannell: Yes, that study just came out and fits perfectly although the authors seemed convinced it is folic acid, an epidemiological impossibility as the cure, increasing folic acid fortification in food was instituted in the late 1990s with no decrease in the incidence of autism.
The reason that I am so interested in autism is because I keep getting letters from parents who have given their autistic children adult doses of vitamin D supplements and mother after mother write in and report to me that their child improved. They use terms such as “a switch goes off.” It’s like they have turned a switch. My website includes four or five of those letters.
One mother had three children with autism. She has twin daughters who are eight years old. She became pregnant again before she knew her twins had autism. All three of her children have autism; two severely afflicted eight year olds and one less afflicted five year old. After three months of vitamin D supplementation, the mother has seen dramatic improvement.
Passwater: Thanks so much for sharing with us the process for which you elucidated your theory, but by now, I’m sure some of our readers are wondering, “How can vitamin D have an effect on what is considered a genetic disease?
Cannell: Genetic diseases include the failure to properly regulate the genes, and as we’ve discussed a couple of times, vitamin D works by directly regulating about 1,000 human genes, which is about 5% of the human genome. The human genome contains more than 2,700 binding sites for 1,25-hydroxy vitamin D; those binding sites are near genes involved in virtually every known major disease of humans. Virtually every cell in the brain has vitamin D receptors. The receptors control gene expression or how genetic material is used. Therefore, vitamin D may have many beneficial effects for the brain. Without vitamin D, those genes literally do not know what to do. They don’t know whether to increase or decrease the production of their particular enzyme or other protein. Vitamin D can turn a gene on or off. The genes don’t perform correctly without vitamin D.
Passwater: While we’re at it, let’s discuss the conventional wisdom that considers autism a genetic disease. Hasn’t a recent study shown that even though there is a large genetic component in that several gene variants have been associated with autism, that there is a larger environmental (non-genetic) factor than previously thought. Here, the use of the word “environmental” includes nutritional factors and possibly metal toxins. (Hallmayer et al. online July 4 in the Archives of General Psychiatry.)
Cannell: Yes, A study of twins in California downgrades the role genes play in autism identifying a large environmental role.
Passwater: Your theory suggests that vitamin D deficiency is an indirect “trigger” to produce autism, whatever the direct cause or causes of autism may be. Does your theory recognize or include any other possible triggers of autism as well. (and if so, would vitamin D still be of benefit if there were other possible triggers?)Cannell: Yes, anything that would stress the immune system like toxins or infections so toxic doses of mercury would be a trigger.
Passwater: Would vitamin D be of help even when the trigger involves other immune system stresses?
Cannell: Yes, vitamin D make the immune system smarter. Autoimmune disorders are, by definition, the result of dumber immune systems.
Passwater: If vitamin D deficiency is a trigger for autism, could vitamin D supplements become a treatment option for children who have already developed autism? You report that vitamin D supplementation in sufficient dose has improved existing cases of autism. So it’s not too late to modify any genetic predisposition to autism even after autism symptoms appear. How long is that window of opportunity? Is there a period of time after which it would be just too late for vitamin D supplementation to help?
Cannell: Autism is an ongoing, destructive, inflammatory autoimmune type of brain disorder that injures the brain. The sooner the vitamin D deficiency is treated, the more likely the child will have a more normal life!
Passwater: What if the child is seven years old and has been diagnosed as autistic for six years? Is that too late?
Cannell: First of all, everything I am saying is simply my observations from unscientific data. I can’t publish these case reports because they are not my patients. I can’t document that these kids actually improved. I can only document that the mothers told me they improved. I have set up a free clinic in the next several months in which I will be able to see children with autism and consult with their parents about vitamin D needs and get the children on the right amount of vitamin D. In addition, a study is underway at the major medical school (UCSF) giving high doses of D to autistic children. This study needs another $9,000 to be completed and another $80,000 if a controlled trial seems indicated from the open study. Those who give may well be able to say they helped fund the seminal study in autism.
Passwater: Still the activist, especially for the poor and under-privileged, I see.
Cannell: In September 2011, the Vitamin D Council began this free clinic for children with autism. My time is free, the autism assessment scales are free, the blood tests are free, and the vitamin D for the kids is free (due to the generosity of Ddrops). We estimate 3-4 clinic visits will be needed. Anyone in the world with a child with autism can call and get an appointment to see me. The Vitamin D Council will sponsor this clinic as long as we can afford it, which means as long as we have enough donors, members and especially enough lifetime members. From now on, a lifetime membership also means that such membership sponsors one autistic child to come to the free clinic and we will encourage that family (if the donor wants) to call and thank the donor in person.
We are taking a risk, as our financial situation is – as it is too often – precarious. In order to have a free clinic we must hire an administrative assistant to organize and help with the free clinic. At this time, I am unable to get a salary from the Vitamin D Council for my time. However, we still have to pay a full time web director, a science advisor, a controller, and a commitment to fund the preliminary study on autism and vitamin D by the University of California at San Francisco. It would be nice if our readers would consider donating or joining as a member. Please remember that our newsletter is free no matter if you join or not. (www.vitamindcouncil.org)
Passwater: It is positively a good cause that can help improve the lives of so many people. But, let’s go back and clarify a point. Right now, would you suggest to the mother of any autistic child that correcting the child’s vitamin D level would be a positive step?
Cannell: There’s no scientific evidence yet published that suggests that vitamin D would have a treatment effect in autism. However, as the person who first proposed the theory, it is my belief that vitamin D does have a treatment effect on autism and I base this solely on what parents are telling me. I further predict that the treatment effect will by modulated by several factors; the more severely affected the child, the less likely there will be a significant treatment effect, secondly, the older the child, the less likely there will be a significant treatment effect. The more vitamin A or cod liver oil the less likely the effect. However, if I had an autistic child who was 25 years old, I would make sure his or her vitamin D level was adequate. That’s the other key thing about autism. For reasons that are entirely unclear to me, autistic children need to have vitamin D levels that are in the high range of normal in order to show improvement.
Passwater: Perhaps, we can go back to your analogy about the lower mountain pools being fed from the higher mountain lakes. Only when the higher lakes overflow will the lower lakes and pools be fed. The vitamin D levels have to be at least high enough to supply adequate vitamin D to the less prioritized needs. Or maybe it just requires more molecules of vitamin D to overcome the greater number of genetic abnormality or polymorphism.
Cannell: That’s right, it must be. I’ve seen that when the mothers give their child a couple thousand IU of vitamin D and their 25-hydroxy vitamin D blood levels get up to 40 or 50 ng/ml, the mothers will say that there is a little improvement, but when I suggest 6,000 IU per day, and the child takes that and a month later, the child’s blood level is up to 80 ng/ml, then the mother is saying, “Wow!”
For autistic children, I like to get their blood levels up to about 100 ng/ml. For many children that takes up to 10,000 IU of vitamin D daily.
Passwater: Your elucidation of the connection between vitamin D deficiency and autism is a very important medical contribution. Let’s pause here until next month when we will chat about vitamin D deficiency and heart disease research.
Dr. Cannell, once again thank you for sharing your knowledge of vitamin D and health with us, and for your many contributions across several health fields, but particularly for your elucidation of the connections between vitamin D deficiency and influenza, autism and the three A’s childhood diseases of modern civilization.
Newly Discovered Effects of Vitamin D on Cancer
An Interview with Professor John H. White, Ph.D.
By Richard A. Passwater, Ph.D.
Vitamin D slows the progression of cells from premalignant to malignant states, keeping their proliferation in check. A team of researchers at McGill University has discovered a molecular basis for the potential cancer-preventive effects of vitamin D (1). The team, led by McGill professors John White and David Goltzman, of the Faculty of Medicine’s department of physiology, discovered that the active form of vitamin D acts by several mechanisms to inhibit both the production and function of a protein that drives cell division and is active at elevated levels in more than half of all cancers.
The initial observation that vitamin D deficiency increases the risk of many cancers, especially breast and colon cancers, was made in the 1970s by brother epidemiologists, Cedric Garland, Ph.D., and Frank Garland, Ph.D. (2). When I wrote my book on cancer and nutrition in 1978, I included five of the mortality maps from National Cancer Institute’s Atlas of Cancer Mortality for U. S. Counties from 1950–1969 to illustrate the epidemiological evidence observed by the Drs. Garland about sunlight exposure (latitude) and cancer incidence.
Vitamin D was thought of only in terms of bone health for decades. It was realized that vitamin D was not a classical vitamin because classical vitamins are part of specific coenzyme systems. Vitamin E is another example of a nonclassical vitamin in that it can act as a general antioxidant. Vitamin D, when converted in the body to its biologically active form has hormone-like actions. Vitamin D has become very sexy in the last five years because it has been found to be involved in many biological pathways and a deficiency increases the risk of many diseases. Much of this research stems from the findings of John H. White, Ph.D., as he has elucidated how vitamin D interacts with more than 1,000 genes.
Professor White, who obtained his Ph.D. in 1987 from Harvard, is a molecular biologist and molecular geneticist who has made numerous broad-ranging contributions to the fields of gene regulation and vitamin D physiology. His work on the molecular mechanisms of vitamin D action opened up the field of study of vitamin D as an inducer of antimicrobial innate immunity in humans, and has provided fundamental insights into its potential role as a cancer chemopreventive agent. Dr. White is a professor in the departments of physiology and medicine at McGill University in Montreal, Canada.
Passwater: Dr. White, congratulations on your recent article published in the Proceedings of the National Academy of Sciences explaining how vitamin D works to regulate cell division (1). This is an extremely important research finding. Why did you become a molecular geneticist in the first place? What drew you to molecular genetics?
White: Molecular biology introduced me to molecular genetics. I became interested in molecular biology as a Ph.D. student. Molecular biology is not a scientific discipline like biochemistry or physiology, but rather a series of elegant molecular techniques for studying biochemistry, physiology and other related fields. Many of these techniques are gene-based; so-called “recombinant DNA technology” and “gene therapy” are components of the molecular biology arsenal, for example.
Passwater: Why did you become interested in gene regulation?
White: Molecular biology introduced me to genes and how they are regulated. As you know, genes encode the information necessary to build proteins. For non-scientist readers to understand what that means, one has to take a step back and understand what cells are.
Cells are units of life, from simple unicellular organisms to complex multicellular ones like humans. It is helpful to imagine that a cell is like a city or city-state. While proteins contribute to the infrastructure of the cell, they are above all like the specialized individuals who make the city work, with all of the specialized tasks that entails. Some of these jobs (e.g., police, bus drivers) are common to all cities, while certain types of expertise (e.g., specialized types of engineers or scientists) are found only in selected areas. Similarly, cells in the liver or, say, the brain will produce common proteins while others will be specific to each cell type. Thus, protein production is specific to the function of a given cell to some degree.
All of this means that protein production must be carefully regulated. The first and, I believe most important, point of this regulation is the control of the first step: gene transcription. Although it is not evident at this point of the conversation, this is highly relevant to how vitamin D works at the molecular level.
Passwater: That’s a nice analogy. How did vitamin D enter your research picture? Were you aware of other research on vitamin D and cancer first, or was it your awareness of vitamin D and genes that came first?
White: The awareness of vitamin D and genes came first, although it took me a while to get there. When I finished my Ph.D., I went to work in a lab that studied how estrogen worked—but not physiologically. The lab had no particular interest in female reproductive function, for example, but rather in the nitty-gritty details of how estrogen worked at the molecular level.
Many readers are aware that estrogen is a steroid hormone. Steroid hormones are small molecules that can freely enter cells. Estrogen acts by binding to a specific protein called the estrogen receptor, which is found in an inner compartment of the cell called the nucleus. The nucleus contains the cell’s DNA (i.e., its genes). Steroid hormone receptors function as “gene switches” and regulate the process, gene transcription, mentioned previously. Estrogen physiology is thus manifested by estrogen’s control of the production of specific proteins through gene transcription in specific cells that are necessary for the menstrual cycle, bone health and more.
Similarly, the active form of vitamin D (commonly called 1,25-dihydroxyvitamin D or calcitriol) binds to a specific receptor, the vitamin D receptor, which regulates the transcription of specific genes. The active form of vitamin D is four metabolic steps removed from cholesterol, another well-known but non-hormonal steroid. The physiological effects of vitamin D thus arise through the regulation of gene transcription. Vitamin D was discovered for its capacity to regulate the body’s uptake and use of calcium, in particular its role in maintaining normal bone health.
My interest in vitamin D was piqued in the late 1990s by a colleague who mentioned in passing that the application of vitamin D to cancers cells grown in tissue culture arrested their division. This so-called “non-classical” action of vitamin D became a main focus of my lab because I realized that I could apply my expertise in studying how estrogen worked to the study of vitamin D.
Passwater: You have identified about 1,000 genes regulated by vitamin D. That is an absolutely amazing feat that has changed our understanding of vitamin D and health. Was the effect of vitamin D on genes known before you identified them? Was vitamin D still looked upon in classical vitamin terms when you started your vitamin D/gene research?
White: In the late 1990s, there was increasing awareness of the non-classical actions of vitamin D and accumulating population-based studies linking vitamin D deficiency with increased rates of specific types of cancers. However, the molecular details of these actions were definitely lacking. I think it is fair to say that my lab was the first to take a comprehensive approach to try and understand these actions by determining on as large a scale as possible the identity of the genes regulated by vitamin D. Before that point, we were aware of only a handful of genes under the control of vitamin D.
Passwater: What was your first important finding in this aspect of your research?
White: That’s a difficult question to answer. Perhaps, in retrospect, the first important finding was what didn’t happen, that vitamin D and the vitamin D receptor were not strongly stimulating the production of a protein that acted as a brake on cell division. We saw lots of changes in gene transcription that were consistent with cell division being arrested. However, the vast majority of these corresponded to the loss of production of proteins necessary for cell division. Moreover, and this is important, we couldn’t tell which changes were a product of the arrest in cell division and which ones were driving it. It took us seven or eight years to begin to figure it out.
As an aside, I should point out that one of the early products of our approach of large-scale identification of vitamin D “target” genes was the realization that vitamin D also controlled the function of the immune system and its primary responses to infection (3). This is one of the fortunate and serendipitous aspects of research, and led to another major research effort in the lab. However, as I said before, the control of cell division by vitamin D was a tougher nut to crack.
Passwater: Wow! The mechanism by which vitamin D regulates the primary response to infection is another outstanding discovery. But, don’t let me interrupt you, where did you go from there regarding elucidating the mechanism for vitamin D regulation of cell division?
White: We came to realize that many of genes whose transcription was reduced in vitamin D-treated cells were also regulated by a protein called cMYC. cMYC is at the same time similar to the vitamin D receptor and in some ways the opposite of it. It is similar in that, like the receptor, cMYC is a regulator of specific genes’ transcription. However, it is the opposite in the sense that, while vitamin D working through its receptor acts to block cell division, cMYC acts to stimulate it. Not surprisingly, the function of cMYC is elevated in about 50% of all cancers, which are of course diseases of uncontrolled cell division.
Slowly, in retrospect perhaps too slowly, it dawned on us that the vitamin D receptor was acting by directly controlling cMYC function. What came as such a surprise, and I think that this is why our paper is important, is that vitamin D and the vitamin D receptor control cMYC function by multiple mechanisms. They depress the rate of transcription of the gene encoding cMYC and thus the production of new cMYC protein. In addition, they increase the rate of degradation, or turnover, of existing cMYC protein. Moreover, they have opposite effects on the production and turnover of a protein called MXD1 that antagonizes cMYC function, leading to dramatic swings in the relative amounts of cMYC and MXD1 in vitamin D-treated cells. This is why we called the vitamin D receptor a “master regulator” of cMYC function in the title of the paper.
Passwater: Is this like putting a brake on runaway cell division or cancer?
White: We think that vitamin D’s control of cMYC function is one of the key elements of its capacity to control cell division and we believe that it represents an important aspect of its anticancer properties. I should point out by “anticancer” I mean the prevention of cancer development, not the treatment of existing cancers. As you know, as cancers progress they can become resistant to various types of therapeutic approaches, and vitamin D treatment is no exception. One day, we would like to understand the mechanisms of resistance to vitamin D of late-stage cancers.
Passwater: Yes, I agree that cancer cells are a different beast and develop their own defense mechanisms. I find a recently published article particularly disturbing (4). The researchers suggest that only one in 10,000 tumor cells may be responsible for keeping a cancer growing. Your research focuses on cancer prevention, however, it hasn’t been shown that controlling cMYC regulation will not put a brake on some cancers. Nor has it been shown that vitamin D will not affect other vitamin D-regulated mechanisms involved in the multi-step DINOMIT theory of cancer.
Vitamin D is incredibly inexpensive, safe and doesn’t interfere with any cancer treatment. I would like to see your findings about cancer prevention tested in cancer patients as well as studied for the prevention of cancer. In the meantime, your findings do suggest that if people maintain adequate levels of vitamin D, their risks of many cancers can be reduced. If people don’t develop cancer in the first place, the need for destroying cancer cells becomes mute.
I have been following the tumor suppressor protein p53 and cancer for about 30 years. Does cMYC fit into the p53 regulatory mechanism?
White: It’s not something that we have been looking at. However, there is some evidence linking elevated transcription of the gene encoding cMYC to chromosomal instability resulting from mutations in p53.
Passwater: Getting back to your findings, how are vitamin D and vitamin A involved in co-regulating genes?
White: The active form of vitamin A in most tissues is retinoic acid. Retinoic acid binds to a receptor related to the vitamin D receptor and thus also functions as a “gene switch.” Like vitamin D, retinoic acid can also regulate cell division. That being said, the extent to which vitamin D and retinoic acid can coregulate gene transcription has not been studied in great detail, but is probably rather limited.
Passwater: We often discuss the relationship between dietary vitamin D (cholecalciferol) and the form of vitamin D that circulates in the blood (25-hydroxy vitamin D or calcidiol) in this column. What blood levels of vitamin D should people have to optimize cMYC regulation?
White: We didn’t look at the levels of vitamin D in the blood in the animal studies. The major circulating form of vitamin D in animals and humans (commonly called 25-hydroxy vitamin D) is a precursor of the active form (1,25-dihydroxyvitamin D). We treated the skin of normal mice with pharmacological concentrations of the active form of vitamin D and saw that levels of cMYC were reduced, effectively reproducing what we saw with human cells propagated in tissue culture. Otherwise, we compared the levels of cMYC in normal mice and mice that could not produce vitamin D receptor, in other words in mice where vitamin D could not function. We saw elevated cMYC production in the skin and colon of “vitamin D defective” mice.
Passwater: How are your findings being received by the scientific community?
White: The results were presented at a workshop on vitamin D function held in Houston last summer and were well received. The paper was also voted one of the top 10 research achievements of 2012 by the Canadian Cancer Society.
Passwater: Where does your research go from here? What are your other research interests in your lab?
White: We are pursuing our vitamin D work on two fronts. We are trying to determine how vitamin D regulates cMYC stability. This may be important, as its stability is controlled by mechanisms that also regulate the stability of a host of other proteins that, like cMYC, act to drive cells through cell division; cMYC in other words may represent the tip of an iceberg in terms of vitamin D action. We are also continuing our work on how vitamin D stimulates cellular responses to bacterial infection.
Passwater: Dr. White, thank you for your discoveries and for chatting with us about their meaning. WF
References
- R. Salehi-Tabar et al., “Vitamin D Receptor as a Master Regulator of the C-MYC/MXD1 Network,” Proc. Nat. Acad. Sci. USA 109 (46), 18827–18832 (2012).
- C.F. Garland and F.C. Garland, “Do Sunlight and Vitamin D Reduce the Likelihood of Colon Cancer?” Int. J. Epidemiol. (3), 227–231 (1980).
- T.T. Wang et al., “Cutting Edge: 1,25-dihydroxyvitamin D3 Is a Direct Inducer of Antimicrobial Peptide Gene Expression,” J. Immunol.173,2909–2912 (2012).
- A. Kreso et al., “Variable Clonal Repopulation Dynamics Influence Chemotherapy Response in Colorectal Cancer,” Science Dec. 13, 2012. [Epub ahead of print].
Where to Buy:
- Vitamin K2 (in MK-9 form) 500mcg x 1000 tablets for £7.86 + £36.99 Shipping = £44.85 = US$72.72
- Vitamin D3 (10,000 IU) x 360 Softgels for US$19.70 + FREE Shipping
—> Coupon for 15% off at pureformulas.com: WLCBEJN115
Action Step / Dosage:
Remember Vitamin D3 & Vitamin K2 need to be taken together — the recommended ratio is:
For every 1000 IU of D3, take 100-200mcg of K2 (in the form of MK-7 or higher [MK-9])
I like to get their Vitamind D3 blood levels up to about 100-120 ng/ml. For many people that takes from 10,000 IU (up to 20,000 IU) of vitamin D3 daily. The best way to determine if your blood levels are high enough is to get your blood tested.
For Daily Usage:
If taking 10,000 IU of Vitamin D3 —-> |
take 1,000 to 2,000 mcg of Vitamin K2 (in form of MK-7 or higher [MK-9]) |
If taking 20,000 IU of Vitamin D3 —-> |
take 2,000 to 4,000 mcg of Vitamin K2 (in form of MK-7 or higher [MK-9]) |
Personally, I am taking 50,000 IU of Vitamin D3 daily for approximately 100 days (with 5,000-10,000 mcg of Vitamin K2 daily) — after this period, I will drop my daily Vitamin D3 intake to about 10,000 IU (and may bring levels back up to 20,000 IU periodically)
For more information about large doses of Vitamin D3 (25,000 > 50,000 > 100,000 IU Daily!) — check out:
The Miraculous Results Of Extremely High Doses Of The Sunshine Hormone Vitamin D3 My Experiment With Huge Doses Of D3 From 25,000 To 50,000 To 100,000 Iu A Day Over A 1 Year Period
Interview with Jeff T. Bowles (interviewer uses some coarse language, but this is an otherwise great interview)
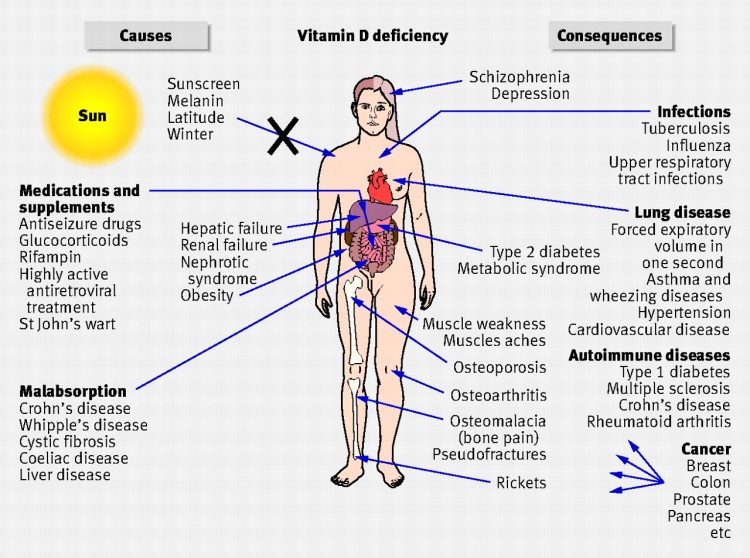


Discussion
Trackbacks/Pingbacks
Pingback: All About Juicing (vegetables) | Make Better Habits - June 17, 2015